Beyond Significance: A Practical Guide to Equivalence Testing for Model Performance in Drug Development
This article provides a comprehensive guide for researchers and drug development professionals on applying equivalence tests to evaluate model performance.
Beyond Significance: A Practical Guide to Equivalence Testing for Model Performance in Drug Development
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on applying equivalence tests to evaluate model performance. Moving beyond traditional null-hypothesis significance testing, we explore the foundational concepts of equivalence testing, including the Two One-Sided Tests (TOST) procedure and the critical role of equivalence bounds. The methodological section delves into advanced approaches like model averaging to handle model uncertainty, while the troubleshooting section addresses common pitfalls such as inflated Type I errors and strategies for power analysis. Finally, we cover validation frameworks aligned with emerging regulatory standards like ICH M15, offering a complete roadmap for demonstrating model comparability in biomedical research and regulatory submissions.
Why Equivalence? Moving Beyond Traditional Significance Testing
In model performance equivalence research, a common misconception is that a statistically non-significant result (p > 0.05) proves two models are equivalent. This article explains the logical fallacy behind this assumption and introduces equivalence testing as a statistically sound alternative for demonstrating similarity, complete with protocols and analytical frameworks for researchers and drug development professionals.
The Fundamental Misinterpretation of Non-Significant Results
What p > 0.05 Actually Means
In standard null hypothesis significance testing (NHST), a p-value greater than 0.05 indicates that the observed data do not provide strong enough evidence to reject the null hypothesis, which typically states that no difference exists (e.g., no difference in model performance) [1] [2]. Critically, this outcome only tells us that we cannot reject the null hypothesis; it does not allow us to accept it or claim the effects are identical [3] [4].
The American Statistical Association (ASA) warns against misinterpreting p-values, stating, "Do not believe that an association or effect is absent just because it was not statistically significant" [4]. A non-significant p-value can result from several factors unrelated to true equivalence:
- High Variance: Noisy data can obscure real differences [1].
- Small Sample Size: Studies with insufficient power may fail to detect meaningful differences that actually exist [1] [5].
The Logical Fallacy: Absence of Evidence vs. Evidence of Absence
Interpreting p > 0.05 as proof of equivalence confuses absence of evidence for a difference with evidence of absence of a difference [3]. As one source notes, "A conclusion does not immediately become 'true' on one side of the divide and 'false' on the other" [4]. In model comparison, failing to prove models are different is not the same as proving they are equivalent.
Core Principles of Equivalence Testing
Equivalence testing directly addresses the need to demonstrate similarity by flipping the conventional testing logic. In equivalence testing:
- The null hypothesis (Hâ‚€) states that the difference between two models is meaningfully large (i.e., lies outside a pre-defined equivalence margin) [5] [6].
- The alternative hypothesis (Hâ‚) states that the difference is trivial (i.e., lies within the equivalence margin) [5].
Rejecting the null hypothesis in this framework provides direct statistical evidence for equivalence, a claim that NHST cannot support [6].
Defining the Equivalence Region
The cornerstone of a valid equivalence test is the equivalence region (also called the "region of practical equivalence" or "smallest effect size of interest") [3] [5]. This is a pre-specified range of values within which differences are considered practically meaningless. The bounds of this region (ΔL and ΔU) should be justified based on:
- Clinical or practical relevance [5] [7]
- Domain expertise and prior knowledge [7]
- Risk assessment (e.g., high-risk scenarios require narrower margins) [7]
For example, in bioequivalence studies for generic drugs, a common equivalence margin is 20%, leading to an acceptance range of 0.80 to 1.25 for the ratio of geometric means [8].
Key Methodological Approaches and Protocols
The Two One-Sided Tests (TOST) Procedure
The most common method for equivalence testing is the Two One-Sided Tests (TOST) procedure [3] [5] [8]. This approach tests whether the observed difference is simultaneously greater than the lower equivalence bound and smaller than the upper equivalence bound.
Experimental Protocol: TOST Procedure
- Pre-specify Equivalence Margin: Define ΔL (lower bound) and ΔU (upper bound) based on practical significance before data collection [5] [7].
- Calculate Test Statistics: Perform two one-sided t-tests:
- Test 1: TL = (M₠- M₂ - ΔL) / (SE)
- Test 2: TU = (M₠- M₂ - ΔU) / (SE) where M₠and M₂ are group means, and SE is the standard error [3].
- Evaluate Significance: If both tests yield p-values < 0.05, reject the null hypothesis of non-equivalence and conclude equivalence [5] [8].
- Confirm with Confidence Intervals: The 90% confidence interval for the difference should lie entirely within the equivalence bounds [5] [8].
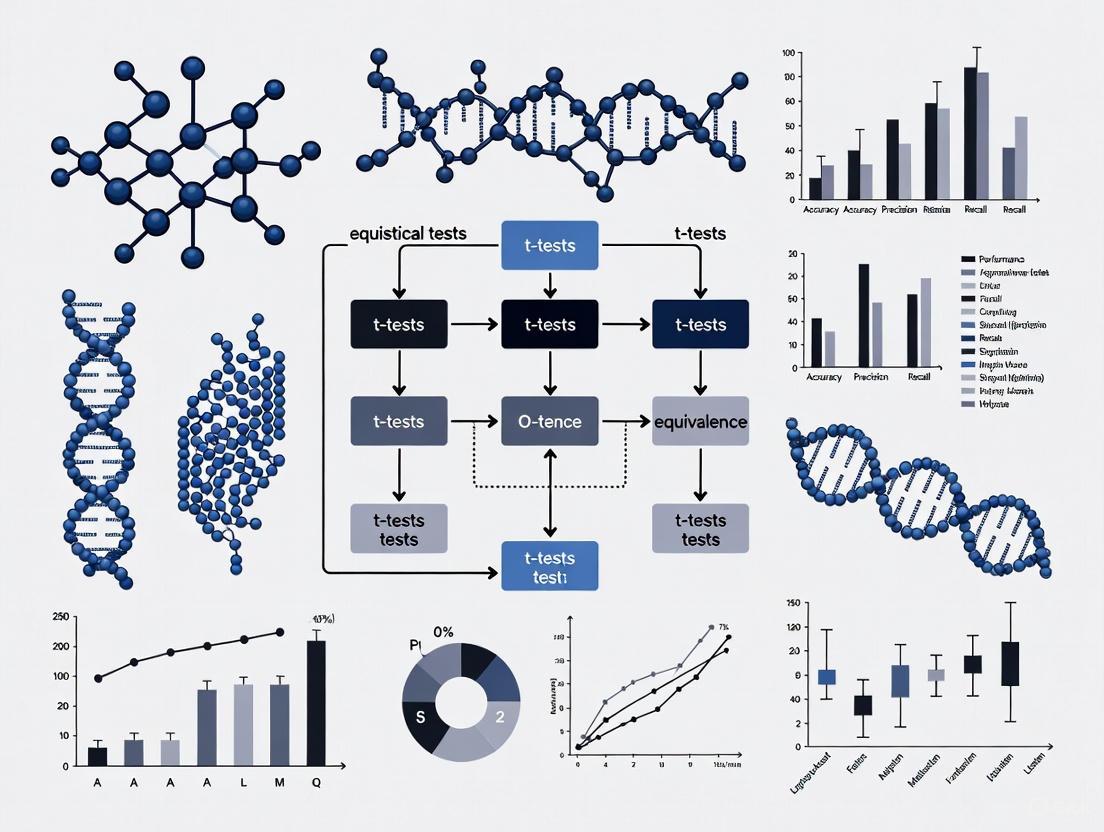
The following diagram illustrates the TOST procedure logic and decision criteria:
Confidence Interval Approach
An alternative but complementary view uses confidence intervals:
- Calculate a 90% confidence interval for the difference between measures [5]
- If the entire confidence interval falls within the pre-specified equivalence bounds, equivalence is demonstrated at the 5% significance level [5]
This approach is visually intuitive and provides additional information about the precision of the estimate.
Practical Applications and Experimental Design
Applications in Model Performance Research
Equivalence testing is particularly valuable in several research scenarios:
- Method Comparison Studies: Demonstrating that a new, cheaper, or faster model performs equivalently to an established gold standard [5]
- Replication Studies: Testing whether a new study replicates a previous finding by showing effects are equivalent within a reasonable margin [3]
- Reliability Assessments: Establishing test-retest reliability by showing measurements taken at different times are equivalent [6]
Regulatory and Industry Applications
In pharmaceutical development and regulatory science, equivalence testing is well-established:
- Bioequivalence Studies: Generic drugs must demonstrate equivalent pharmacokinetic parameters to brand-name drugs [8]
- Biosimilarity Assessment: Biological products must show they are highly similar to reference products despite minor differences [8]
- Process Change Validation: Manufacturing process changes require demonstration of equivalent product quality attributes [7]
Essential Research Reagent Solutions
The table below outlines key methodological components for implementing equivalence testing in research practice:
| Component | Function | Implementation Example |
|---|---|---|
| Equivalence Margin | Defines the range of practically insignificant differences | Pre-specified as ±Δ based on clinical relevance or effect size conventions [5] |
| TOST Framework | Provides statistical test for equivalence | Two one-sided t-tests with null hypotheses of non-equivalence [3] [8] |
| Power Analysis | Determines sample size needed to detect equivalence | Sample size calculation ensuring high probability of rejecting non-equivalence when true difference is small [7] |
| Confidence Intervals | Visual and statistical assessment of equivalence | 90% CI plotted with equivalence bounds; complete inclusion demonstrates equivalence [5] |
| Sensitivity Analysis | Tests robustness of conclusions to margin choices | Repeating analysis with different equivalence margins to ensure conclusions are consistent [5] |
Complete Experimental Workflow for Equivalence Testing
The following diagram outlines the comprehensive workflow for designing, executing, and interpreting an equivalence study:
The misinterpretation of p > 0.05 as proof of equivalence represents a significant logical and statistical error in model performance research. Equivalence testing, particularly through the TOST procedure, provides a rigorous methodological framework for demonstrating similarity when that is the research objective. By pre-specifying clinically meaningful equivalence bounds and using appropriate statistical techniques, researchers can make valid claims about equivalence that stand up to scientific and regulatory scrutiny.
In statistical hypothesis testing, particularly in equivalence and non-inferiority research, the Smallest Effect Size of Interest (SESOI) represents the threshold below which effect sizes are considered practically or clinically irrelevant. Unlike traditional significance testing that examines whether an effect exists, equivalence testing investigates whether an effect is small enough to be considered negligible for practical purposes. The SESOI is formalized through predetermined equivalence bounds (denoted as Δ or -ΔL to ΔU), which create a range of values considered practically equivalent to the null effect. Establishing appropriate equivalence bounds enables researchers to statistically reject the presence of effects substantial enough to be meaningful, thus providing evidential support for the absence of practically important effects [9].
The specification of SESOI marks a paradigm shift from merely testing whether effects are statistically different from zero to assessing whether they are practically insignificant. This approach addresses a critical limitation of traditional null hypothesis significance testing, where non-significant results (p > α) are often misinterpreted as evidence for no effect, when in reality the test might simply lack statistical power to detect a true effect [9] [3]. Within the frequentist framework, the Two One-Sided Tests (TOST) procedure has emerged as the most widely recommended method for testing equivalence, where an upper and lower equivalence bound is specified based on the SESOI [9].
Theoretical Foundations and Statistical Framework
The TOST Procedure and Interval Hypotheses
The Two One-Sided Tests (TOST) procedure, developed in pharmaceutical sciences and later formalized for broader applications, provides a straightforward method for equivalence testing [9] [3]. In this procedure, two composite null hypotheses are tested: H01: Δ ≤ -ΔL and H02: Δ ≥ ΔU, where Δ represents the true effect size. Rejecting both null hypotheses allows researchers to conclude that -ΔL < Δ < ΔU, meaning the observed effect falls within the equivalence bounds and is practically equivalent to the null effect [9].
The TOST procedure fundamentally changes the structure of hypothesis testing from point null hypotheses to interval hypotheses. Rather than testing against a nil null hypothesis of exactly zero effect, equivalence tests evaluate non-nil null hypotheses that represent ranges of effect sizes deemed importantly different from zero [3]. This approach aligns statistical testing more closely with scientific reasoning, as researchers are typically interested in rejecting effect sizes large enough to be meaningful rather than proving effects exactly equal to zero [9] [3].
Table 1: Comparison of Statistical Testing Approaches
| Testing Approach | Null Hypothesis | Alternative Hypothesis | Scientific Question | ||||
|---|---|---|---|---|---|---|---|
| Traditional NHST | Effect = 0 | Effect ≠0 | Is there any effect? | ||||
| Equivalence Test | Effect | ≥ Δ | Effect | < Δ | Is the effect negligible? | ||
| Minimum Effect Test | Effect | ≤ Δ | Effect | > Δ | Is the effect meaningful? |
Interpreting Results from Equivalence Tests
When combining traditional null hypothesis significance tests (NHST) with equivalence tests, four distinct interpretations emerge from study results [9]:
- Statistically equivalent and not statistically different from zero: The 90% confidence interval around the observed effect excludes the equivalence bounds, while the 95% confidence interval includes zero.
- Statistically different from zero but not statistically equivalent: The 95% confidence interval excludes zero, but the 90% confidence interval includes at least one equivalence bound.
- Statistically different from zero and statistically equivalent: Both the 90% confidence interval excludes the equivalence bounds and the 95% confidence interval excludes zero.
- Undetermined: Neither statistically different from zero nor statistically equivalent.
This refined classification enables more nuanced statistical conclusions than traditional dichotomous significant/non-significant outcomes.
Practical Approaches for Setting Equivalence Bounds
Methodological Frameworks for Determining SESOI
Establishing appropriate equivalence bounds requires careful consideration of contextual factors. Several established approaches guide researchers in determining the SESOI [9]:
- Clinical or practical significance: In medical research, bounds may be based on the Minimal Clinically Important Difference (MCID), representing the smallest difference patients or clinicians would consider important [10].
- Theoretical predictions: When theories make precise predictions about effect sizes, bounds can be set based on theoretically meaningful thresholds.
- Resource constraints: When theoretical or practical boundaries are absent, researchers may set bounds based on the smallest effect size they have sufficient power to detect given available resources [9].
- Field-specific conventions: Some domains have established standards, such as the 80%-125% bioequivalence criterion used in pharmaceutical research [11] [12].
The equivalence bound can be symmetric around zero (e.g., ΔL = -0.3 to ΔU = 0.3) or asymmetric (e.g., ΔL = -0.2 to ΔU = 0.4), depending on the research context and consequences of positive versus negative effects [9].
Standardized Effect Size Benchmarks
For psychological and social sciences where raw effect sizes lack intuitive interpretation, setting bounds based on standardized effect sizes (e.g., Cohen's d, η²) facilitates comparison across studies using different measures [9]. Common benchmarks include:
Table 2: Common Standardized Effect Size Benchmarks for Equivalence Bounds
| Effect Size Metric | Small Effect | Medium Effect | Large Effect | Typical Equivalence Bound |
|---|---|---|---|---|
| Cohen's d | 0.2 | 0.5 | 0.8 | ±0.2 to ±0.5 |
| Correlation (r) | 0.1 | 0.3 | 0.5 | ±0.1 to ±0.2 |
| Partial η² | 0.01 | 0.06 | 0.14 | 0.01 to 0.04 |
For ANOVA models, equivalence bounds can be set using partial eta-squared (η²p) values, representing the proportion of variance explained. Campbell and Lakens (2021) recommend setting bounds based on the smallest proportion of variance that would be considered theoretically or practically meaningful [13].
Regulatory and Domain-Specific Standards
In pharmaceutical research and bioequivalence studies, stringent standards have been established through regulatory guidance. The 80%-125% rule is widely accepted for bioequivalence assessment, based on the assumption that differences in systemic exposure smaller than 20% are not clinically significant [11] [12]. This criterion requires that the 90% confidence intervals of the ratios of geometric means for pharmacokinetic parameters (AUC and Cmax) fall entirely within the 80%-125% range after logarithmic transformation [11].
For drugs with a narrow therapeutic index or high intra-subject variability, regulatory agencies may require stricter equivalence bounds or specialized statistical approaches such as reference-scaled average bioequivalence with replicated crossover designs [11]. The European Medicines Agency (EMA) emphasizes that equivalence margins should be justified through a combination of empirical evidence and clinical judgment, considering the smallest difference that would warrant disregarding a novel intervention in favor of a criterion standard [10] [14].
Experimental Protocols and Implementation
The TOST Procedure: A Step-by-Step Protocol
Implementing equivalence testing using the TOST procedure involves these methodical steps [9] [3]:
Define equivalence bounds: Before data collection, specify lower and upper equivalence bounds (-ΔL and ΔU) based on the SESOI, considering clinical, theoretical, or practical implications.
Collect data and compute test statistics: Conduct the study using appropriate experimental designs (e.g., crossover, parallel groups) with sufficient sample size determined through power analysis.
Perform two one-sided tests:
- Test H01: Δ ≤ -ΔL using t-statistic:
- Test H02: Δ ≥ ΔU using t-statistic: Where M1 and M2 are group means, and SE is the standard error of the difference.
Evaluate p-values: Obtain p-values for both one-sided tests. If both p-values are less than the chosen α level (typically 0.05), reject the composite null hypothesis of meaningful effect.
Interpret confidence intervals: Alternatively, construct a 90% confidence interval for the effect size. If this interval falls completely within the equivalence bounds (-ΔL to ΔU), conclude equivalence.
Figure 1: TOST Procedure Workflow for Equivalence Testing
Sample Size Planning and Power Analysis
Power analysis for equivalence tests requires special consideration, as standard power calculations for traditional tests are inadequate. When planning equivalence studies, researchers should [9]:
- Conduct power analyses specifically designed for equivalence tests
- Determine sample size needed to reject both null hypotheses when the true effect is zero
- Consider that equivalence tests generally require larger sample sizes than traditional tests to achieve comparable power
- Account for the specified equivalence bounds in power calculations, with narrower bounds requiring larger samples
For F-test equivalence testing in ANOVA designs, power analysis involves calculating the non-centrality parameter based on the equivalence bound and degrees of freedom [13]. The TOSTER package in R provides specialized functions for power analysis of equivalence tests, enabling researchers to determine required sample sizes for various designs [13].
Regulatory Considerations for Clinical Trials
In clinical trial design, particularly for non-inferiority and equivalence trials, the estimands framework (ICH E9[R1]) provides a structured approach to defining treatment effects [14]. Key considerations include:
- Handling intercurrent events: Post-baseline events that affect endpoint interpretation (e.g., treatment discontinuation) must be addressed using appropriate strategies (treatment policy, hypothetical, composite, etc.)
- Dual estimand approach: Regulatory agencies often recommend defining two co-primary estimands using different strategies for handling intercurrent events [14]
- Maintaining blinding: Equivalence trials should maintain blinding to prevent biased assessment of endpoints
- Prespecification: All aspects of equivalence testing, including bounds, analysis methods, and handling of intercurrent events, must be specified before data collection
Comparison of Equivalence Testing Approaches
Domain-Specific Applications and Standards
Equivalence testing methodologies vary across research domains, reflecting differing needs and regulatory requirements:
Table 3: Comparison of Equivalence Testing Approaches Across Domains
| Research Domain | Primary Metrics | Typical Equivalence Bounds | Regulatory Guidance | Special Considerations |
|---|---|---|---|---|
| Pharmacokinetics/Bioequivalence | AUC, Cmax ratios | 80%-125% (log-transformed) | FDA, EMA, ICH guidelines | Narrow therapeutic index drugs require stricter bounds |
| Clinical Trials (Non-inferiority) | Clinical endpoints | Based on MCID and prior superiority effects | EMA, FDA guidance | Choice of estimand for intercurrent events critical |
| Psychology/Social Sciences | Standardized effect sizes (Cohen's d, η²) | ±0.2 to ±0.5 SD units | APA recommendations | Often lack consensus on meaningful effect sizes |
| Manufacturing/Quality Control | Process parameters | Based on functional specifications | ISO standards | Often one-sided equivalence testing |
Advanced Methodological Variations
Beyond the standard TOST procedure, several advanced equivalence testing methods have been developed:
- Non-inferiority tests: One-sided tests examining whether an intervention is not substantially worse than a comparator [10]
- Minimum effect tests: Tests that reject effect sizes smaller than a specified minimum value, establishing that an effect is both statistically and practically significant [3]
- Empirical Equivalence Bound (EEB): A data-driven approach that estimates the minimum equivalence bound that would lead to equivalence when equivalence is true [15]
- Bayesian equivalence methods: Approaches that use Bayesian statistics to evaluate evidence for equivalence
For ANOVA models, equivalence testing can be extended to omnibus F-tests using the non-central F distribution. The test evaluates whether the total proportion of variance attributable to factors is less than the equivalence bound [13].
Statistical Software and Implementation Tools
Several specialized tools facilitate implementation of equivalence tests:
Table 4: Essential Resources for Equivalence Testing
| Tool/Resource | Function | Implementation | Key Features |
|---|---|---|---|
| TOSTER Package | Equivalence tests for t-tests, correlations, meta-analyses | R, SPSS, Spreadsheet | User-friendly interface, power analysis |
| equ_ftest() Function | Equivalence testing for F-tests in ANOVA | R (TOSTER package) | Handles various ANOVA designs, power calculation |
| B-value Calculation | Empirical equivalence bound estimation | Custom R code | Data-driven bound estimation |
| Power Analysis Tools | Sample size determination for equivalence tests | R (TOSTER), PASS, G*Power | Specialized for equivalence testing needs |
| Regulatory Guidance Documents | Protocol requirements for clinical trials | FDA, EMA websites | Domain-specific standards and requirements |
Reporting Guidelines and Best Practices
When reporting equivalence tests, researchers should:
- Clearly justify the chosen equivalence bounds based on clinical, theoretical, or practical considerations
- Report both traditional significance tests and equivalence test results
- Include confidence intervals alongside point estimates
- Document power calculations and sample size justifications
- For clinical trials, specify estimands and strategies for handling intercurrent events
- Use appropriate visualizations to display equivalence test results
Figure 2: Interpreting Equivalence Test Results Using Confidence Intervals
Setting appropriate equivalence bounds based on the Smallest Effect Size of Interest represents a fundamental advancement in statistical practice, enabling researchers to draw meaningful conclusions about the absence of practically important effects. The TOST procedure provides a statistically sound framework for implementing equivalence tests across diverse research domains, from pharmaceutical development to social sciences. By carefully considering clinical, theoretical, and practical implications when establishing equivalence bounds, and following rigorous experimental protocols, researchers can produce more informative and clinically relevant results. As methodological developments continue to emerge, including empirical equivalence bounds and Bayesian approaches, the statistical toolkit for equivalence testing will further expand, enhancing our ability to demonstrate when differences are negligible enough to be disregarded for practical purposes.
In scientific research, particularly in fields like drug development and psychology, researchers often need to demonstrate the absence of a meaningful effect rather than confirm its presence. Equivalence testing provides a statistical framework for this purpose, reversing the traditional logic of null hypothesis significance testing (NHST). While NHST aims to reject the null hypothesis of no effect, equivalence testing allows researchers to statistically reject the presence of effects large enough to be considered meaningful, thereby providing support for the absence of a practically significant effect [9].
This comparative guide examines the Two One-Sided Tests (TOST) procedure, the most widely recommended approach for equivalence testing within a frequentist framework. We will explore its statistical foundations, compare it with traditional significance testing, provide detailed experimental protocols, and demonstrate its application across various research contexts, with particular emphasis on pharmaceutical development and model performance evaluation.
TOST Procedure: Core Concepts and Statistical Framework
Foundational Principles
The TOST procedure operates on a different logical framework than traditional hypothesis tests. Instead of testing against a point null hypothesis (e.g., μ₠- μ₂ = 0), TOST evaluates whether the true effect size falls within a predetermined range of practically equivalent values [9] [16].
The procedure establishes an equivalence interval defined by lower and upper bounds (ΔL and ΔU) representing the smallest effect size of interest (SESOI). These bounds specify the range of effect sizes considered practically insignificant, often symmetric around zero (e.g., -0.3 to 0.3 for Cohen's d) but potentially asymmetric in applications where risks differ in each direction [9] [7].
The statistical hypotheses for TOST are formulated as:
- Null hypothesis (H₀): The true effect is outside the equivalence bounds (Δ ≤ -ΔL or Δ ≥ ΔU)
- Alternative hypothesis (Hâ‚): The true effect is within the equivalence bounds (-ΔL < Δ < ΔU) [9] [16]
Operational Mechanism
TOST decomposes the composite null hypothesis into two one-sided tests conducted simultaneously:
- Test 1: H₀¹: Δ ≤ -ΔL versus H₹: Δ > -ΔL
- Test 2: H₀²: Δ ≥ ΔU versus H₲: Δ < ΔU [16]
Equivalence is established only if both one-sided tests reject their respective null hypotheses at the chosen significance level (typically α = 0.05 for each test) [9]. This dual requirement provides strong control over Type I error rates, ensuring the probability of falsely claiming equivalence does not exceed α [16].
Table 1: Key Components of the TOST Procedure
| Component | Description | Considerations |
|---|---|---|
| Equivalence Bounds | Pre-specified range (-ΔL to ΔU) of practically insignificant effects | Should be justified based on theoretical, clinical, or practical considerations [9] |
| Two One-Sided Tests | Simultaneous tests against lower and upper bounds | Each test conducted at significance level α (typically 0.05) [16] |
| Confidence Interval | 100(1-2α)% confidence interval (e.g., 90% CI when α=0.05) | Equivalence concluded if entire CI falls within equivalence bounds [9] [17] |
| Decision Rule | Reject non-equivalence if both one-sided tests are significant | Provides strong control of Type I error at α [16] |
TOST Versus Traditional Significance Testing
Conceptual and Practical Differences
TOST and traditional NHST address fundamentally different research questions, leading to distinct interpretations and conclusions, particularly in cases of non-significant results.
Table 2: Comparison Between Traditional NHST and TOST Procedure
| Aspect | Traditional NHST | TOST Procedure |
|---|---|---|
| Research Question | Is there a statistically significant effect? | Is the effect practically insignificant? |
| Null Hypothesis | Effect size equals zero | Effect size exceeds equivalence bounds |
| Alternative Hypothesis | Effect size does not equal zero | Effect size falls within equivalence bounds |
| Interpretation of p > α | Inconclusive ("no evidence of an effect") | Cannot claim equivalence [9] |
| Type I Error | Concluding an effect exists when it doesn't | Concluding equivalence when effects are meaningful [18] |
| Confidence Intervals | 95% CI; significance if excludes zero | 90% CI; equivalence if within bounds [9] [17] |
Interpreting Different Outcomes
The relationship between TOST and NHST leads to four possible conclusions in research findings [9]:
- Statistically equivalent and not statistically different from zero: The 90% CI falls entirely within equivalence bounds, and the 95% CI includes zero
- Statistically different from zero but not statistically equivalent: The 95% CI excludes zero, but the 90% CI exceeds equivalence bounds
- Statistically different from zero and statistically equivalent: The 90% CI falls within bounds, and the 95% CI excludes zero (possible with high precision)
- Undetermined: Neither statistically different from zero nor statistically equivalent
This nuanced interpretation framework prevents the common misinterpretation of non-significant NHST results as evidence for no effect [9].
Establishing Equivalence Bounds and Experimental Protocols
Determining the Smallest Effect Size of Interest
Setting appropriate equivalence bounds represents one of the most critical aspects of TOST implementation. Three primary approaches guide this process:
- Theoretical justification: Bounds based on established minimal important differences in the field
- Practical considerations: Bounds reflecting cost-benefit tradeoffs or risk assessments
- Resource-based approach: When theoretical boundaries are absent, bounds can be set to the smallest effect size researchers have sufficient power to detect given available resources [9]
In pharmaceutical applications, equivalence bounds often derive from risk-based assessments considering potential impacts on process capability and out-of-specification rates [7]. For instance, shifting a critical quality attribute by a certain percentage (e.g., 10-25%) may be evaluated for its impact on failure rates, with higher-risk attributes warranting narrower bounds [7].
Statistical Implementation Protocol
The following step-by-step protocol outlines the TOST procedure for comparing a test product to a standard reference, a common application in pharmaceutical development [7]:
Step 1: Define Equivalence Bounds
- Identify the reference standard and its target value
- Conduct risk assessment to establish upper and lower practical limits (UPL and LPL)
- Justify bounds based on scientific knowledge, product experience, and clinical relevance
- Example: For pH with USL=8 and LSL=7, medium risk might justify bounds of ±0.15 (15% of tolerance) [7]
Step 2: Determine Sample Size
- Conduct power analysis to ensure adequate sensitivity
- Use formula for one-sided tests: n = (tâ‚₋α + tâ‚₋β)²(s/δ)²
- Account for the dual one-sided testing structure (α typically 0.05 for each test)
- Example: Minimum sample size of 13 with target of 15 for medium effect [7]
Step 3: Data Collection and Preparation
- Collect measurements according to predefined experimental design
- Calculate differences from standard reference value
- Verify data quality and assumptions
Step 4: Statistical Analysis
- Perform two one-sided t-tests against LPL and UPL
- Calculate p-values for both tests:
- pL = P(t ≥ (x̄ - LPL)/(s/√n))
- pU = P(t ≤ (x̄ - UPL)/(s/√n)) [7]
- Construct 90% confidence interval around mean difference
Step 5: Interpretation and Conclusion
- If both p-values < 0.05 (and 90% CI within bounds), conclude equivalence
- Report results with confidence intervals and justification for equivalence bounds
- If equivalence not demonstrated, conduct root-cause analysis [7]
Applications in Pharmaceutical Development and Model Evaluation
Bioequivalence and Comparability Studies
TOST has extensive applications in pharmaceutical development, particularly in bioequivalence trials where researchers aim to demonstrate that two drug formulations have similar pharmacokinetic properties [18]. Regulatory agencies like the FDA require 90% confidence intervals for geometric mean ratios of key parameters (e.g., AUC, Cmax) to fall within [0.8, 1.25] to establish bioequivalence [16].
In comparability studies following manufacturing process changes, TOST provides statistical evidence that product quality attributes remain equivalent pre- and post-change [7]. This application is crucial for regulatory submissions, as highlighted in FDA's guidance on comparability protocols [7].
Clinical Trial Applications
Equivalence trials in clinical research aim to show that a new intervention is not unacceptably different from a standard of care, potentially offering advantages in cost, toxicity, or administration [18]. For example:
- McCann et al. tested equivalence in neurodevelopment between anesthesia types, defining equivalence as ≤5 point difference in IQ scores [18]
- Marzocchi et al. established equivalence between tirofiban and abciximab with a 10% margin for ST-segment resolution [18]
These applications demonstrate how TOST facilitates evidence-based decisions about treatment alternatives while controlling error rates.
Implementation Tools and Visualization
Software and Computational Tools
While early adoption of equivalence testing in psychology was limited by software accessibility [9], dedicated packages now facilitate TOST implementation:
- R packages: The
TOSTERpackage provides comprehensive functions for t-tests, correlations, and meta-analyses [19] - Spreadsheet implementations: User-friendly calculators for common equivalence tests [9]
- Statistical software: Commercial packages like JMP and Minitab include equivalence testing modules
The t_TOST() function in R performs three tests simultaneously: the traditional two-tailed test and two one-sided equivalence tests, providing comprehensive results in a single operation [20].
Visual Representation of TOST Logic
The following diagram illustrates the decision framework for the TOST procedure, showing the relationship between confidence intervals and equivalence conclusions:
This decision framework illustrates how the combination of TOST and traditional testing leads to nuanced conclusions about equivalence and difference, addressing the limitation of traditional NHST in supporting claims of effect absence [9].
Table 3: Key Resources for Implementing Equivalence Tests
| Resource Category | Specific Tools/Solutions | Function/Purpose |
|---|---|---|
| Statistical Software | R with TOSTER package [19] |
Comprehensive equivalence testing implementation |
| Sample Size Calculators | Power analysis tools for TOST [9] | Determining required sample size for target power |
| Equivalence Bound Justification | Risk assessment frameworks [7] | Establishing scientifically defensible bounds |
| Data Visualization | Consonance plots [20] | Visual representation of equivalence test results |
| Regulatory Guidance | FDA/EMA bioequivalence standards [16] | Defining equivalence criteria for specific applications |
The TOST procedure represents a fundamental advancement in statistical methodology, enabling researchers to make scientifically rigorous claims about effect absence rather than merely failing to detect differences. Its logical framework, based on simultaneous testing against upper and lower equivalence bounds, provides strong error control while addressing a question of profound practical importance across scientific disciplines.
For model performance evaluation and pharmaceutical development, TOST offers particular value in comparability assessments, bioequivalence studies, and method validation. By specifying smallest effect sizes of interest based on theoretical or practical considerations, researchers can design informative experiments that advance scientific knowledge beyond the limitations of traditional significance testing.
As methodological awareness increases and software implementation becomes more accessible, equivalence testing is poised to become an standard component of the statistical toolkit, promoting more nuanced and scientifically meaningful inference across research domains.
Bioequivalence (BE) assessment serves as a critical regulatory pathway for approving generic drug products, founded on the principle that demonstrating comparable drug exposure can serve as a surrogate for demonstrating comparable therapeutic effect [12]. According to the U.S. Code of Federal Regulations (21 CFR Part 320), bioavailability refers to "the extent and rate to which the active drug ingredient or active moiety from the drug product is absorbed and becomes available at the site of drug action" [21]. When two drug products are pharmaceutical equivalents or alternatives and their rates and extents of absorption show no significant differences, they are considered bioequivalent [12].
This concept forms the Foundation of generic drug approval under the Drug Price Competition and Patent Term Restoration Act of 1984, which allows for Abbreviated New Drug Applications (ANDAs) that do not require lengthy clinical trials for safety and efficacy [12]. The Fundamental Bioequivalence Assumption states that "if two drug products are shown to be bioequivalent, it is assumed that they will generally reach the same therapeutic effect or they are therapeutically equivalent" [12]. This regulatory framework has made cost-effective generic therapeutics widely available, typically priced 80-85% lower than their brand-name counterparts [11].
Regulatory Framework and Guidelines
FDA Statistical Approaches to Bioequivalence
The U.S. Food and Drug Administration's (FDA) 2001 guidance document "Statistical Approaches to Establishing Bioequivalence" provides recommendations for sponsors using equivalence criteria in analyzing in vivo or in vitro BE studies for Investigational New Drugs (INDs), New Drug Applications (NDAs), ANDAs, and supplements [22]. This guidance discusses three statistical approaches for comparing bioavailability measures: average bioequivalence, population bioequivalence, and individual bioequivalence [22].
The FDA's current regulatory framework requires pharmaceutical companies to establish that test and reference formulations are average bioequivalent, though distinctions exist between prescribability (where either formulation can be chosen for starting therapy) and switchability (where a patient can switch between formulations without issues) [23]. For regulatory approval, evidence of BE must be submitted in any ANDA, with certain exceptions where waivers may be granted [21].
Types of Bioequivalence Studies
Table 1: Approaches to Bioequivalence Assessment
| Approach | Definition | Regulatory Status |
|---|---|---|
| Average Bioequivalence (ABE) | Formulations are equivalent with respect to means of their probability distributions | Currently required by USFDA [23] |
| Population Bioequivalence (PBE) | Formulations equivalent with respect to underlying probability distributions | Discussed in FDA guidance [22] |
| Individual Bioequivalence (IBE) | Formulations equivalent for large proportion of individuals | Discussed in FDA guidance [22] |
ICH Guidelines and Global Harmonization
Substantial efforts for global harmonization of bioequivalence requirements have been undertaken through initiatives like the Global Bioequivalence Harmonization Initiative (GBHI) and the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) [11]. One significant development is the ICH M9 guideline, which addresses the Biopharmaceutical Classification System (BCS)-based biowaiver concept, allowing waivers for in vivo bioequivalence studies under certain conditions based on drug solubility and permeability [11].
Harmonization efforts focus on several key areas, including selection criteria for reference products among regulatory agencies to reduce the need for repetitive BE studies, and requirements for waivers for BE studies [11]. These international harmonization initiatives aim to streamline global drug development while maintaining rigorous standards for therapeutic equivalence.
Statistical Foundations of Bioequivalence Testing
Hypothesis Testing in Equivalence Trials
Unlike superiority trials that aim to detect differences, equivalence trials test the null hypothesis that differences between treatments exceed a predefined margin [18]. The statistical formulation for average bioequivalence testing is structured as:
- Null Hypothesis (H₀): μT/μR ≤ Ψ₠or μT/μR ≥ Ψ₂
- Alternative Hypothesis (Hâ‚): Ψ₠< μT/μR < Ψ₂
where μT and μR represent population means for test and reference formulations, and Ψ₠and Ψ₂ are equivalence margins set at 0.80 and 1.25, respectively, for pharmacokinetic parameters like AUC and Cmax [23].
The type 1 error (false positive) in equivalence trials is the risk of falsely concluding equivalence when treatments are actually not equivalent, typically set at 5% [18]. This means we need 95% confidence that the treatment difference does not exceed the equivalence margin in either direction.
Confidence Interval Approach
The standard analytical approach for bioequivalence assessment uses the confidence interval method [18]. For average bioequivalence, the 90% confidence interval for the ratio of geometric means of the primary pharmacokinetic parameters must fall entirely within the bioequivalence limits of 80% to 125% [11]. This is typically implemented using:
- The Two One-Sided Tests (TOST) procedure, which employs two one-sided tests with 5% significance levels each, corresponding to a two-sided 90% confidence interval [18]
- Alternatively, a single two-sided test with 5% significance level, corresponding to a two-sided 95% confidence interval [18]
The following diagram illustrates the logical decision process for bioequivalence assessment using the confidence interval approach:
Figure 1: Bioequivalence Statistical Decision Pathway
Logarithmic Transformation
Pharmacokinetic parameters like AUC and Cmax typically follow lognormal distributions rather than normal distributions [23]. Applying logarithmic transformation achieves normal distribution of the data and creates symmetry in the equivalence criteria [11]. On the logarithmic scale, the bioequivalence range of 80-125% becomes -0.2231 to 0.2231, which is symmetric around zero [11]. After statistical analysis on the transformed data, results are back-transformed to the original scale for interpretation.
Experimental Design and Methodologies
Standard Bioequivalence Study Designs
The FDA recommends crossover designs for bioavailability studies unless parallel or other designs are more appropriate for valid scientific reasons [12]. The most common experimental designs include:
- Two-period, two-sequence, two-treatment, single-dose crossover design: The most commonly used design where each subject receives both test and reference formulations in randomized sequence with adequate washout periods [11]
- Single-dose parallel design: Used when crossover designs are not feasible due to long half-lives or other considerations
- Replicate design: Employed for highly variable drugs or specific regulatory requirements, allowing estimation of within-subject variability [11]
For certain products intended for EMA submission, a multiple-dose crossover design may be used to assess steady-state conditions [11].
Key Pharmacokinetic Parameters
Table 2: Primary Pharmacokinetic Parameters in Bioequivalence Studies
| Parameter | Definition | Physiological Significance | BE Assessment Role |
|---|---|---|---|
| AUC₀–t | Area under concentration-time curve from zero to last measurable time point | Measure of total drug exposure (extent of absorption) | Primary endpoint for extent of absorption [11] |
| AUC₀–∞ | Area under concentration-time curve from zero to infinity | Measure of total drug exposure accounting for complete elimination | Primary endpoint for extent of absorption [11] |
| Cmax | Maximum observed concentration | Measure of peak exposure (rate of absorption) | Primary endpoint for rate of absorption [11] |
| Tmax | Time to reach Cmax | Measure of absorption rate | Supportive parameter; differences may require additional analyses [11] |
Subject Selection and Ethical Considerations
BE studies are generally conducted in individuals at least 18 years old, who may be healthy volunteers or specific patient populations for which the drug is intended [11]. The use of healthy volunteers rather than patients is based on the assumption that bioequivalence in healthy subjects is predictive of therapeutic equivalence in patients [12]. Sample size determination considers the equivalence margin, type I error (typically 5%), and type II error (typically 80-90% power), with requirements generally larger than superiority trials due to the small equivalence margins [18].
Bioequivalence Criteria and Statistical Analysis
The 80-125% Rule
The current international standard for bioequivalence requires that the 90% confidence intervals for the ratio of geometric means of both AUC and Cmax must fall entirely within 80-125% limits [11]. This criterion was established based on the assumption that differences in systemic exposure smaller than 20% are not clinically significant [11]. The following diagram illustrates various possible outcomes when comparing confidence intervals to equivalence margins:
Figure 2: Confidence Interval Scenarios for Bioequivalence
Analysis of Variance in Crossover Designs
For standard 2x2 crossover studies, statistical analysis typically employs analysis of variance (ANOVA) models that account for sequence, period, and treatment effects [23]. The mixed-effects model includes:
- Fixed effects: Formulation, period, sequence
- Random effect: Subject within sequence
The FDA recommends logarithmic transformation of AUC and Cmax before analysis, with results back-transformed to the original scale for presentation [23]. Both intention-to-treat and per-protocol analyses should be presented, as intention-to-treat analysis may minimize differences and potentially lead to erroneous conclusions of equivalence [18].
Special Cases and Methodological Adaptations
Highly Variable Drugs
For drugs with high within-subject variability (intra-subject CV > 30%), standard bioequivalence criteria may require excessively large sample sizes [11]. Regulatory agencies have developed adapted approaches such as reference-scaled average bioequivalence that scale the equivalence limits based on within-subject variability of the reference product [11].
Narrow Therapeutic Index Drugs
For drugs with narrow therapeutic indices (e.g., warfarin, digoxin), where small changes in blood concentration can cause therapeutic failure or severe adverse events, stricter bioequivalence criteria have been proposed [11]. These may include tighter equivalence limits (e.g., 90-111%) or replicated study designs that allow comparison of both means and variability [11].
Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Methodologies in Bioequivalence Studies
| Reagent/Solution | Function | Application Context |
|---|---|---|
| Validated Bioanalytical Methods | Quantification of drug concentrations in biological matrices | Essential for measuring plasma/serum concentration-time profiles [11] |
| Stable Isotope-Labeled Internal Standards | Normalization of extraction efficiency and instrument variability | Liquid Chromatography-Mass Spectrometry (LC-MS/MS) bioanalysis [11] |
| Clinical Protocol with Crossover Design | Controlled administration of test and reference formulations | 2x2 crossover or replicated designs to minimize between-subject variability [23] [11] |
| Pharmacokinetic Modeling Software | Calculation of AUC, Cmax, Tmax, and other parameters | Non-compartmental analysis of concentration-time data [23] |
| Statistical Analysis Software | Implementation of ANOVA, TOST, and confidence interval methods | SAS, R, or other validated platforms for BE statistical analysis [23] |
Practical Implementation and Case Study
Example Bioequivalence Assessment
A practical example from a 2×2 crossover bioequivalence study with 28 healthy volunteers illustrates the implementation process [23]. The study measured AUC and Cmax for test and reference formulations, with natural logarithmic transformation applied before statistical analysis. The analysis yielded the following results:
Table 4: Example Bioequivalence Study Results
| Parameter | Estimate for ln(μR/μT) | Estimate for μR/μT | 90% CI for μR/μT | BE Conclusion |
|---|---|---|---|---|
| AUC | 0.0893 | 1.09 | (0.89, 1.34) | Not equivalent (CI exceeds 1.25) |
| Cmax | -0.104 | 0.90 | (0.75, 1.08) | Not equivalent (CI below 0.80) |
In this case, neither parameter's 90% confidence interval fell entirely within the 80-125% range, so bioequivalence could not be concluded, and the FDA would not approve the generic product based on this study [23].
Common Methodological Pitfalls
Several common issues can compromise bioequivalence studies:
- Inadequate sample size: Underpowered studies may fail to demonstrate equivalence even when products are truly equivalent [18]
- Inappropriate subject population: Healthy volunteers may not represent patients for certain drug classes
- Protocol deviations: Poor compliance, vomiting, or dropouts can reduce evaluable data
- Analytical issues: Lack of assay validation or poor precision can introduce variability
- Incorrect statistical analysis: Failure to use appropriate models or account for period effects
Bioequivalence trials represent a specialized application of equivalence testing principles within pharmaceutical regulation, with well-established statistical and methodological frameworks. The current approach centered on average bioequivalence with 80-125% criteria has successfully ensured therapeutic equivalence of generic drugs while promoting competition and accessibility.
Ongoing harmonization initiatives through ICH and other international bodies continue to refine and standardize bioequivalence requirements across jurisdictions. Future developments may include greater acceptance of model-based bioequivalence approaches, further refinement of methods for highly variable drugs, and potential expansion of biowaiver provisions based on the Biopharmaceutical Classification System.
For researchers designing equivalence studies in other domains, the rigorous framework developed for bioequivalence assessment offers valuable insights into appropriate statistical methods, study design considerations, and regulatory standards for demonstrating therapeutic equivalence without undertaking large-scale clinical endpoint studies.
Implementing Equivalence Tests: From TOST to Advanced Model Averaging
A Guide to Statistical Tests for Model Performance Equivalence
In model performance evaluation, a non-significant result from a traditional null hypothesis significance test (NHST) is often—and incorrectly—interpreted as evidence of equivalence. The Two One-Sided T-Test (TOST) procedure rectifies this by providing a statistically rigorous framework to confirm the absence of a meaningful effect, establishing that differences between models are practically insignificant [9] [5]. This guide details the protocol for conducting a TOST, complete with experimental data and workflows, to objectively assess model equivalence in research and development.
Understanding the TOST Procedure
The TOST procedure is a foundational method in equivalence testing. Unlike traditional t-tests that aim to detect a difference, TOST is designed to confirm the absence of a meaningful difference by testing whether the true effect size lies within a pre-specified range of practical equivalence [24] [9].
- Core Hypotheses: In TOST, the roles of the null and alternative hypotheses are reversed from traditional testing.
- Null Hypothesis (Hâ‚€): The effect is outside the equivalence bounds (i.e., a meaningful difference exists). Formally, this is stated as ( H{01}: \theta \leq -\Delta ) or ( H{02}: \theta \geq \Delta ), where ( \theta ) is the population parameter (e.g., mean difference) and ( \Delta ) is the equivalence margin [24] [3].
- Alternative Hypothesis (Hâ‚): The effect is inside the equivalence bounds (i.e., no meaningful difference). Formally, ( -\Delta < \theta < \Delta ) [24].
- The TOST Method: To test these hypotheses, TOST performs two one-sided tests [24] [5]:
- Test if the effect is greater than the lower bound (( -\Delta )).
- Test if the effect is less than the upper bound (( \Delta )). If both tests are statistically significant, the null hypothesis is rejected, and we conclude equivalence.
Research Reagent Solutions
The table below details the essential components for designing and executing a TOST analysis.
| Item | Function in TOST Analysis |
|---|---|
| Statistical Software (R/Python/SAS) | Provides computational environment for executing two one-sided t-tests and calculating confidence intervals. The TOSTER package in R is a dedicated toolkit [19]. |
| Pre-Specified Equivalence Margin ((\Delta)) | A pre-defined, context-dependent range ([(-\Delta, \Delta)]) representing the largest difference considered practically irrelevant. This is the most critical reagent [5] [3]. |
| Dataset with Continuous Outcome | The raw data containing the continuous performance metrics (e.g., accuracy, MAE) of the two models or groups being compared. |
| Power Analysis Tool | Used prior to data collection to determine the minimum sample size required to have a high probability of declaring equivalence when it truly exists [9]. |
Experimental Protocol for a Two-Sample TOST
This protocol outlines the steps to test the equivalence of means between two independent groups, such as two different machine learning models.
Step 1: Define the Equivalence Margin Before collecting data, define the smallest effect size of interest (SESOI), which sets your equivalence margin, (\Delta) [9] [3]. This margin must be justified based on domain knowledge, clinical significance, or practical considerations. For example, in bioequivalence studies for drug development, a common margin for log-transformed parameters is ([log(0.8), log(1.25)]) [16]. For standardized mean differences (Cohen's d), bounds of -0.5 and 0.5 might be used [24].
Step 2: Formulate the Hypotheses Set up your statistical hypotheses based on the pre-defined margin.
- Hâ‚€: The true mean difference ( \mu1 - \mu2 \leq -\Delta ) or ( \mu1 - \mu2 \geq \Delta ). (The models are not equivalent.)
- Hâ‚: The true mean difference ( -\Delta < \mu1 - \mu2 < \Delta ). (The models are equivalent.)
Step 3: Calculate the Test Statistics and P-values Conduct two separate one-sided t-tests. For each test, you will calculate a t-statistic and a corresponding p-value [24] [17].
- Test 1 (vs. the lower bound): ( t1 = \frac{(\bar{X}1 - \bar{X}2) - (-\Delta)}{sp \sqrt{\frac{1}{n1} + \frac{1}{n2}}} ) where ( \bar{X} ) is the sample mean, ( n ) is the sample size, and ( s_p ) is the pooled standard deviation.
- Test 2 (vs. the upper bound): ( t2 = \frac{(\bar{X}1 - \bar{X}2) - \Delta}{sp \sqrt{\frac{1}{n1} + \frac{1}{n2}}} )
Step 4: Make a Decision Based on the P-values The overall p-value for the TOST procedure is the larger of the two p-values from the one-sided tests [5] [17]. If this p-value is less than your chosen significance level (typically ( \alpha = 0.05 )), you reject the null hypothesis and conclude statistical equivalence.
Step 5: Interpret Results Using a Confidence Interval An equivalent and often more intuitive way to interpret TOST is with a 90% Confidence Interval [24] [5]. Why 90%? Because TOST is performed at the 5% significance level for each tail, corresponding to a 90% two-sided CI.
- If the entire 90% confidence interval for the mean difference falls entirely within the equivalence bounds ([-\Delta, \Delta]), you can declare equivalence.
Figure 1: The logical workflow for conducting and interpreting a TOST equivalence test, showing the parallel paths of using p-values and confidence intervals.
Example: Equivalence of Two Model Performances
Suppose you have developed a new, computationally efficient model (Model B) and want to test if its performance is equivalent to your established baseline (Model A). You define the equivalence margin as a difference of 0.5 in Mean Absolute Error (MAE), a practically insignificant amount in your domain.
Experimental Data: After running both models on a test set, you collect the following MAE values:
| Model | Sample Size (n) | Mean MAE | Standard Deviation (s) |
|---|---|---|---|
| Model A | 50 | 10.2 | 1.8 |
| Model B | 50 | 10.4 | 1.9 |
TOST Analysis:
- Equivalence Margin: ( \Delta = 0.5 )
- Observed Mean Difference: ( 10.4 - 10.2 = 0.2 )
- Pooled Standard Deviation: ( s_p \approx 1.85 )
- 90% Confidence Interval for the Difference:
[-0.15, 0.55](hypothetical calculation for illustration). - TOST P-values: The p-value for the test against the lower bound (-0.5) is 0.001; against the upper bound (0.5) is 0.036 [17]. The overall TOST p-value is 0.036.
Interpretation: While the observed difference (0.2) is within the [-0.5, 0.5] margin, the 90% confidence interval [-0.15, 0.55] slightly exceeds the upper bound. Consequently, despite one of the p-values being significant, the TOST procedure would fail to confirm full equivalence because the 90% CI is not entirely contained within the equivalence bounds [24] [5]. This outcome demonstrates the conservativeness and rigor of the TOST method.
TOST vs. Traditional T-Test
The table below summarizes the key philosophical and procedural differences between the two approaches.
| Feature | Traditional NHST T-Test | TOST Equivalence Test |
|---|---|---|
| Null Hypothesis (Hâ‚€) | The means are exactly equal (effect size = 0). | The effect is outside the equivalence bounds (a meaningful difference exists). |
| Alternative Hypothesis (Hâ‚) | The means are not equal (an effect exists). | The effect is within the equivalence bounds (no meaningful difference). |
| Primary Goal | Detect any statistically significant difference. | Establish practical similarity or equivalence. |
| Interpretation of a non-significant p-value | "No evidence of a difference" (but cannot claim equivalence). | Test is inconclusive; cannot claim equivalence [24] [9]. |
| Key Output for Decision | 95% Confidence Interval (checks if it includes 0). | 90% Confidence Interval (checks if it lies entirely within [–Δ, Δ]) [24] [5]. |
Key Considerations for Practitioners
- Justifying the Equivalence Margin: The most critical and often challenging step is choosing a defensible ( \Delta ). This should be based on substantive knowledge, not statistical properties. In model performance, it could be the smallest loss in accuracy that is meaningful to the application [5] [3].
- Power and Sample Size: Equivalence tests require sufficient statistical power to reject the presence of a meaningful effect. A priori power analysis for TOST is essential to ensure your study is informative; underpowered tests will fail to confirm equivalence even if it holds [9] [19].
- One-Sided Tests: Non-Inferiority: Sometimes the research question is only whether a new model is not worse than an existing one by a margin. This is a non-inferiority test, which is a simplified, one-sided version of TOST where you only test against the lower equivalence bound [24] [3].
The TOST procedure empowers researchers in drug development and data science to move beyond simply failing to find a difference and instead build positive evidence for the equivalence of models, treatments, or measurement methods. By rigorously defining an equivalence margin and following the structured protocol outlined above, professionals can generate robust, statistically sound, and practically meaningful conclusions about model performance.
In statistical modeling, particularly in regression analysis, a fundamental challenge is that the true data-generating process is nearly always unknown. This issue, termed model uncertainty, refers to the imperfections and idealizations inherent in every physical model formulation [25]. Model uncertainty arises from simplifying assumptions, unknown boundary conditions, and the effects of variables not included in the model [25]. In practical terms, this means that even with perfect knowledge of input variables, our predictions of system responses will contain uncertainty beyond what comes from the basic input variables themselves [25].
The consequences of ignoring model uncertainty can be severe, leading to overconfident predictions, inflated Type I errors, and ultimately, unreliable scientific conclusions [26]. In high-stakes fields like drug development, where this guide is particularly focused, such overconfidence can translate to costly clinical trial failures or missed therapeutic opportunities. Researchers have broadly categorized uncertainty into two main types: epistemic uncertainty, which stems from a lack of knowledge and is potentially reducible with more data, and aleatoric uncertainty, which represents inherent stochasticity in the system and is generally irreducible [27] [28].
This guide examines contemporary approaches for addressing model uncertainty, with particular emphasis on statistical equivalence testing and model averaging techniques that have shown promise for validating model performance when the true regression model remains unknown.
Quantifying and Classifying Model Uncertainty
Fundamental Classification of Uncertainty
Model uncertainty manifests in several distinct forms, each requiring different handling strategies. The literature generally recognizes three primary classifications of model uncertainty [29]:
- Uncertainty about the true model: This encompasses uncertainty regarding the functional form, distributional assumptions, and relevant variables in the data-generating process.
- Model selection uncertainty: The inherent randomness in model selection results, where different models may be selected from the same data-generating process using different data samples.
- Model selection instability: The phenomenon where slight changes in data lead to significantly different selected models, despite using the same selection procedure.
From a practical perspective, uncertainty is also categorized based on its reducibility [27] [28]:
- Epistemic uncertainty: Arises from limited data or knowledge and can theoretically be reduced with additional information.
- Aleatoric uncertainty: Stems from inherent stochasticity in the system and persists regardless of data quantity.
These uncertainty types collectively contribute to the total predictive uncertainty that researchers must quantify and manage, particularly in regulated environments like pharmaceutical development.
Mathematical Formalization of Model Uncertainty
The discrepancy between model predictions and true system behavior can be formalized as:
[ X{\text{true}} = X{\text{pred}} \times B ]
where (B) represents the model uncertainty, characterized probabilistically through multiple observations and predictions [25]. The mean of (B) expresses bias in the model, while the standard deviation captures the variability of model predictions [25].
In computational terms, the relationship between observations and model predictions can be expressed as:
[ y^e(\mathbf{x}) = y^m(\mathbf{x}, \boldsymbol{\theta}^*) + \delta(\mathbf{x}) + \varepsilon ]
where (y^e(\mathbf{x})) represents experimental observations, (y^m(\mathbf{x}, \boldsymbol{\theta}^)) represents model predictions with calibrated parameters (\boldsymbol{\theta}^), (\delta(\mathbf{x})) represents model discrepancy (bias), and (\varepsilon) represents random observation error [28].
Statistical Frameworks for Handling Model Uncertainty
Equivalence Testing for Model Validation
Traditional hypothesis testing frameworks are fundamentally misaligned with model validation objectives. In standard statistical testing, the null hypothesis typically assumes no difference, placing the burden of proof on demonstrating model inadequacy [30]. Equivalence testing reverses this framework, making the null hypothesis that the model is not valid (i.e., that it exceeds a predetermined accuracy threshold) [30].
The core innovation of equivalence testing is the introduction of a "region of indifference" within which differences between model predictions and experimental data are considered negligible [30]. This region is implemented as an interval around a nominated metric (e.g., mean difference between predictions and observations). If a confidence interval for this metric falls completely within the region of indifference, the model is deemed significantly similar to the true process [30].
Table 1: Comparison of Statistical Testing Approaches for Model Validation
| Testing Approach | Null Hypothesis | Burden of Proof | Interpretation of Non-Significant Result |
|---|---|---|---|
| Traditional Testing | Model is accurate | Prove model wrong | Insufficient evidence to reject (inconclusive) |
| Equivalence Testing | Model is inaccurate | Prove model accurate | Evidence that model meets accuracy standards |
The Two One-Sided Test (TOST) procedure operationalizes this approach by testing whether the mean difference between predictions and observations is both significantly greater than the lower equivalence bound and significantly less than the upper equivalence bound [30]. This method provides a statistically rigorous framework for demonstrating model validity rather than merely failing to demonstrate invalidity.
Model Averaging Approaches
Model averaging has emerged as a powerful alternative to traditional model selection for addressing model uncertainty. Rather than selecting a single "best" model from a candidate set, model averaging incorporates information from multiple plausible models, providing more robust inference and prediction [26].
The primary advantage of model averaging over model selection is its stability—minor changes in data are less likely to produce dramatically different results [26]. This stability is particularly valuable in drug development contexts where decisions have significant financial and clinical implications.
Table 2: Model Averaging Techniques for Addressing Model Uncertainty
| Technique | Basis for Weights | Key Features | Applications |
|---|---|---|---|
| Smooth AIC Weights | Akaike Information Criterion | Frequentist approach; asymptotically equivalent to Mallows CP | General regression modeling |
| Smooth BIC Weights | Bayesian Information Criterion | Approximates posterior model probabilities | Bayesian model averaging |
| FIC Weights | Focused Information Criterion | Optimizes for specific parameter of interest | Targeted inference problems |
| Bayesian Model Averaging | Posterior model probabilities | Fully Bayesian framework; incorporates prior knowledge | Small to moderate sample sizes |
Model averaging is particularly valuable in dose-response studies and time-response modeling, where the true functional form is rarely known with certainty [26]. By combining estimates from multiple candidate models (e.g., linear, quadratic, Emax, sigmoidal), researchers can obtain more reliable inferences while explicitly accounting for model uncertainty.
Experimental Protocols for Evaluating Model Uncertainty
Protocol 1: Equivalence Testing for Regression Curves
Objective: To test whether two regression curves (e.g., from different patient populations or experimental conditions) are equivalent over the entire covariate range.
Methodology:
- Define equivalence threshold: Establish a clinically or scientifically meaningful threshold for the maximum acceptable difference between curves (e.g., Δ = 0.5 on the response scale).
- Select distance measure: Choose an appropriate distance measure between curves, such as the maximum absolute distance ((L_\infty)) or integrated squared difference.
- Calculate confidence interval: Derive a confidence interval for the selected distance measure using appropriate techniques (e.g., bootstrap methods).
- Test equivalence: Compare the confidence interval to the equivalence threshold. If the entire interval falls within [-Δ, Δ], conclude equivalence.
This approach overcomes limitations of traditional methods that test equivalence only at specific points (e.g., mean responses or AUC) rather than across the entire functional relationship [26].
Protocol 2: Model Averaging for Dose-Response Analysis
Objective: To estimate a dose-response relationship while accounting for uncertainty in the functional form.
Methodology:
- Specify candidate models: Identify a set of biologically plausible models (e.g., linear, Emax, sigmoid Emax, exponential).
- Estimate model weights: Compute weights for each model using an information criterion (e.g., AIC, BIC) or Bayesian approach.
- Compute averaged prediction: For any given dose level, compute the weighted average of predictions from all models.
- Quantify uncertainty: Calculate prediction intervals that incorporate both within-model and between-model uncertainty.
This protocol explicitly acknowledges that no single model perfectly represents the true relationship, providing more honest uncertainty quantification [26].
Visualization of Uncertainty Quantification Workflows
Diagram 1: Uncertainty Quantification Workflow for Regression Modeling
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Addressing Model Uncertainty
| Tool | Function | Application Context |
|---|---|---|
| Two One-Sided Tests (TOST) | Tests whether parameter falls within equivalence range | Model validation; bioequivalence assessment |
| Smooth AIC/BIC Weights | Computes model weights for averaging | Multi-model inference and prediction |
| Bayesian Model Averaging (BMA) | Averages models using posterior probabilities | Bayesian analysis with model uncertainty |
| Monte Carlo Dropout | Estimates uncertainty in neural networks | Deep learning applications |
| Deep Ensembles | Combines predictions from multiple neural networks | Uncertainty quantification in deep learning |
| Polynomial Chaos Expansion | Represents uncertainty via orthogonal polynomials | Engineering and physical models |
| Bootstrap Confidence Intervals | Estimates sampling distributions | Non-parametric uncertainty quantification |
Comparative Performance of Uncertainty Quantification Methods
Recent research has systematically evaluated various approaches for handling model uncertainty across different application domains.
Table 4: Performance Comparison of Uncertainty Quantification Methods
| Method | Theoretical Basis | Strengths | Limitations | Computational Demand |
|---|---|---|---|---|
| Equivalence Testing | Frequentist hypothesis testing | Clear decision rule; regulatory acceptance | Requires pre-specified equivalence margin | Low to moderate |
| Model Averaging | Information theory or Bayesian | Robust to model misspecification; incorporates model uncertainty | Weight determination can be sensitive to candidate set | Moderate |
| Bayesian Neural Networks | Bayesian probability | Natural uncertainty representation; principled framework | Computationally intensive; prior specification challenges | High |
| Deep Ensembles | Frequentist ensemble methods | State-of-the-art for many applications; scalable | Multiple training required; less interpretable | High |
| Gaussian Processes | Bayesian nonparametrics | Flexible uncertainty estimates; closed-form predictions | Poor scalability to large datasets | High for large n |
In pharmaceutical applications, studies have demonstrated that model averaging approaches maintain better calibration and predictive performance compared to model selection when substantial model uncertainty exists [26]. Similarly, equivalence testing provides a more appropriate framework for model validation compared to traditional hypothesis testing, particularly in bioequivalence studies and model-based drug development [30].
Model uncertainty presents a fundamental challenge in regression modeling and drug development. By acknowledging that all models are approximations and explicitly quantifying the associated uncertainties, researchers can make more reliable inferences and predictions. The approaches discussed in this guide—particularly equivalence testing and model averaging—provide powerful frameworks for handling model uncertainty in practice.
The choice of method depends on the specific research context, with equivalence testing offering a rigorous approach for model validation against experimental data, and model averaging providing robust inference when multiple plausible models exist. As the field advances, the integration of these approaches with modern machine learning techniques promises to further enhance our ability to quantify and manage uncertainty in complex biological systems.
Leveraging Model Averaging with Smooth BIC Weights for Robust Inference
In scientific research, particularly in fields like drug development and toxicology, statistical inference often faces a fundamental challenge: model uncertainty. When multiple statistical models can plausibly describe the same dataset, relying on a single selected model can lead to overconfident inferences and poor predictive performance. This problem is especially pronounced in dose-response studies, genomics, and risk assessment, where the true data-generating process is complex and imperfectly understood [31] [26].
Model averaging has emerged as a powerful solution to this problem, with smooth BIC weighting representing one of the most rigorous implementations of this approach. Unlike traditional model selection which chooses a single "best" model, model averaging combines estimates from multiple candidate models, thereby accounting for uncertainty in the model selection process itself [32] [33]. This approach recognizes that different models capture different aspects of the truth, and that a weighted combination often provides more robust inference than any single model.
Frequentist model averaging using smooth BIC weights is particularly valuable for equivalence testing and dose-response analysis, where it helps overcome the limitations of model misspecification [26]. By distributing weight across models according to their statistical support, researchers can reduce the influence of high-leverage points that often distort parametric inferences in poorly specified models [34]. This guide provides a comprehensive comparison of model averaging approaches, with particular emphasis on the performance characteristics of smooth BIC weighting relative to competing methods.
Theoretical Foundations: How Model Averaging Mitigates Model Uncertainty
The Framework of Model Averaging
Model averaging operates on a simple but powerful principle: rather than selecting a single model from a candidate set, we combine estimates from all models using carefully chosen weights. For a parameter of interest μ, the model averaging estimate takes the form:
[ \hat{\mu}{MA} = \sum{m=1}^{M} wm \hat{\mu}m ]
where (\hat{\mu}m) is the estimate of μ from model m, and (wm) are weights assigned to each model, with (\sum{m=1}^{M} wm = 1) and (w_m \geq 0) [32]. The theoretical justification for this approach stems from recognizing that model selection introduces additional variability that is typically ignored in post-selection inference [33].
The performance of model averaging critically depends on how the weights are determined. Different weighting schemes have been proposed, including:
- Smooth AIC weights: Based on the Akaike Information Criterion
- Smooth BIC weights: Based on the Bayesian Information Criterion
- Frequentist model averaging: Minimizing Mallows' criterion or using cross-validation
- Bayesian model averaging (BMA): Based on posterior model probabilities [35] [36]
Smooth BIC Weighting Mechanism
Smooth BIC weighting employs the Bayesian Information Criterion to determine model weights. For a set of M candidate models, the weight for model m is calculated as:
[ wm^{BIC} = \frac{\exp(-\frac{1}{2} \Delta BICm)}{\sum{j=1}^{M} \exp(-\frac{1}{2} \Delta BICj)} ]
where (\Delta BICm = BICm - \min(BIC)) is the difference between the BIC of model m and the minimum BIC among all candidate models [26] [32]. The BIC itself is defined as:
[ BICm = -2 \cdot \log(Lm) + k_m \cdot \log(n) ]
where (Lm) is the maximized likelihood value for model m, (km) is the number of parameters, and n is the sample size.
The BIC approximation has strong theoretical foundations in Bayesian statistics, as it approximates the log posterior odds between models under specific prior assumptions [35]. This connection to Bayesian methodology gives smooth BIC weights a solid theoretical justification beyond mere algorithmic convenience.
Table 1: Comparison of Major Model Averaging Weighting Schemes
| Weighting Scheme | Theoretical Basis | Asymptotic Properties | Primary Application Context |
|---|---|---|---|
| Smooth BIC | Bayesian posterior probability approximation | Consistent model selection | Parameter estimation, hypothesis testing |
| Smooth AIC | Kullback-Leibler divergence minimization | Minimax-rate optimal | Prediction-focused applications |
| Bayesian Model Averaging | Formal Bayesian inference with priors | Depends on prior specification | Fully Bayesian analysis contexts |
| Jackknife Model Averaging | Cross-validation performance | Optimal for prediction error | High-dimensional settings, forecasting |
Visualizing the Model Averaging Process with Smooth BIC Weights
The following diagram illustrates the complete workflow for implementing model averaging with smooth BIC weights:
The diagram highlights key advantages of the smooth BIC approach: it automatically penalizes model complexity through the BIC penalty term, provides weights that are proportional to empirical evidence, and delivers a combined estimator that accounts for model uncertainty.
Experimental Protocols: Implementing Model Averaging in Practice
Standard Implementation Protocol
The implementation of model averaging with smooth BIC weights follows a systematic protocol:
Define Candidate Model Set: Identify a scientifically plausible set of candidate models. In dose-response studies, this typically includes linear, quadratic, Emax, sigmoid Emax, and exponential models [26].
Fit Individual Models: Estimate parameters for each candidate model using maximum likelihood or other appropriate estimation techniques.
Compute BIC Values: For each model m, calculate:
- Log-likelihood: ( \log(L_m) )
- Parameter count: ( k_m )
- Sample size: n
- ( BICm = -2 \cdot \log(Lm) + k_m \cdot \log(n) )
Calculate Weights:
- Find minimum BIC: ( BIC{min} = \min(BIC1, BIC2, ..., BICM) )
- Compute differences: ( \Delta BICm = BICm - BIC_{min} )
- Calculate weights: ( wm = \exp(-\frac{1}{2} \Delta BICm) / \sum{j=1}^M \exp(-\frac{1}{2} \Delta BICj) )
Combine Estimates: Compute weighted average of parameter estimates across all models.
Uncertainty Quantification: Estimate variance using appropriate methods such as bootstrap or asymptotic approximations [32] [34].
Experimental Design Considerations
Optimal experimental design for model averaging represents an emerging research area. Studies show that Bayesian optimal designs customized for model averaging can reduce mean squared error by up to 45% compared to traditional designs [31] [33]. These designs account for the fact that different experimental conditions provide varying amounts of information for model discrimination and parameter estimation.
When designing experiments for settings where model averaging will be employed, researchers should:
- Include design points that help discriminate between competing models
- Balance replication across treatment conditions
- Consider optimal allocation of resources to minimize the expected variance of model-averaged estimates [31]
Comparative Performance: Smooth BIC Weights Versus Alternatives
Quantitative Performance Metrics
Table 2: Performance Comparison of Model Averaging Methods in Simulation Studies
| Method | Mean Squared Error Reduction | Type I Error Control | Power for Equivalence Testing | Stability with Small Samples |
|---|---|---|---|---|
| Smooth BIC Weights | 35-45% [31] | Good [26] | High [26] | Moderate |
| Smooth AIC Weights | 25-35% [34] | Acceptable [34] | High [34] | Good |
| Bayesian Model Averaging | 30-40% [35] | Good [35] | Moderate-High [35] | Sensitive to priors |
| Single Model Selection | Reference level | Often inflated [33] | Variable [26] | Poor |
| Frequentist MA (Mallows) | 30-40% [36] | Good [36] | High [36] | Good |
The superior performance of smooth BIC weights in parameter estimation is particularly evident in complex modeling scenarios. In dose-response studies, model averaging with BIC weights demonstrated better calibration and precision compared to model selection approaches [26]. Similarly, in premium estimation for reinsurance losses, BIC-weighted model averaging provided more robust estimates than selecting a single "best" model based on AIC or BIC [32].
Application in Equivalence Testing
Model averaging with smooth BIC weights shows particular promise in equivalence testing, where researchers need to determine whether two regression curves (e.g., from different patient groups or treatments) are equivalent over an entire range of covariate values [26]. Traditional approaches that assume a known regression model can suffer from inflated Type I errors or conservative performance when models are misspecified.
In one comprehensive study, model averaging using smooth BIC weights was applied to test equivalence of time-response curves in toxicological gene expression data. The approach successfully handled model uncertainty across 1000 genes without requiring manual model specification for each gene, demonstrating both computational efficiency and statistical robustness [26].
The following diagram illustrates how model averaging enhances the equivalence testing framework:
Research Reagent Solutions
Table 3: Essential Computational Tools for Model Averaging Implementation
| Tool/Resource | Function | Implementation Considerations |
|---|---|---|
| BIC Calculation | Model evidence quantification | Most statistical software provides built-in BIC computation |
| Weight Normalization | Prevents numerical instability | Use log-sum-exp trick for large model spaces |
| Bootstrap Methods | Variance estimation for MA estimators | 1000+ bootstrap samples recommended for stable intervals |
| Cross-Validation | Alternative weight specification | Computational intensive but useful for predictive tasks |
| Optimal Design Algorithms | Experimental design for MA | Custom algorithms that minimize expected MSE of MA estimates |
Successful implementation of model averaging with smooth BIC weights requires both statistical software and appropriate computational techniques. Most major statistical platforms (R, Python, SAS) include built-in functions for BIC calculation, though custom programming is often needed for the weighting and combination steps.
For variance estimation, bootstrapping has emerged as the most practical approach, particularly for complex models where asymptotic approximations may be unreliable [26] [34]. The bootstrap procedure involves:
- Generating bootstrap resamples from the original data
- Applying the entire model averaging procedure to each resample
- Calculating the variance of the model-averaged estimates across bootstrap samples
This approach accounts for uncertainty from both parameter estimation and model weighting, providing more accurate confidence intervals than methods that condition on a fixed set of weights.
Model averaging with smooth BIC weights represents a statistically rigorous approach to addressing model uncertainty in scientific research. The method's strong theoretical foundations, combined with compelling empirical performance across diverse applications, make it particularly valuable for equivalence testing and dose-response analysis in drug development.
The comparative evidence indicates that smooth BIC weighting typically outperforms both model selection and alternative weighting schemes in terms of mean squared error reduction and inference robustness. The 35-45% MSE reduction achievable with optimally designed experiments represents a substantial efficiency gain that can translate to more reliable scientific conclusions and potentially reduced sample size requirements [31].
For researchers implementing these methods, key recommendations include:
- Carefully select candidate models based on scientific plausibility rather than statistical convenience
- Consider optimal experimental designs when possible to maximize information for model averaging
- Use bootstrap methods for uncertainty quantification rather than relying solely on asymptotic approximations
- Report both model-averaged results and the weights assigned to different models to enhance interpretability
As statistical science continues to evolve, model averaging approaches like smooth BIC weighting are poised to become standard methodology for research areas where model uncertainty cannot be ignored. Their ability to provide more robust inferences while acknowledging the limitations of any single model makes them particularly well-suited for the complex challenges of modern scientific investigation.
In regulatory toxicology and drug development, a common problem is determining whether the effect of an explanatory variable (like a drug dose or time point) on an outcome variable is equivalent across different groups, such as those based on gender, age, or treatment formulations [26]. Equivalence testing provides a powerful statistical framework for these assessments by testing whether the difference between groups does not exceed a pre-specified equivalence threshold [26] [37]. This approach stands in contrast to traditional hypothesis testing, where the goal is to detect differences, and is particularly valuable for bioequivalence studies that investigate whether two formulations of a drug have nearly the same effect and can be considered interchangeable [37].
When comparing effects across groups that vary along a continuous covariate like time or dose, classical approaches that test equivalence of single quantities (e.g., means or area under the curve) often prove inadequate [26]. Instead, researchers have increasingly turned to methods that assess equivalence of whole regression curves over the entire covariate range [26] [37]. These curve-based tests utilize suitable distance measures, such as the maximum absolute distance between two curves, to make more comprehensive equivalence determinations [26].
A critical challenge in implementing these advanced equivalence tests is model uncertainty - the fact that the true underlying regression model is rarely known in practice [26] [37]. Model misspecification can lead to severe problems, including inflated Type I errors or conservative test procedures [37]. This case study explores how model averaging techniques can overcome this limitation while examining time-response curves in toxicological gene expression data, providing researchers with a more robust framework for equivalence assessment.
Methodological Approaches
Traditional Framework for Curve-Based Equivalence Testing
The foundation of curve-based equivalence testing begins with defining appropriate regression models for the response data. In toxicological studies, researchers typically model the relationship between a continuous predictor variable (dose or time) and a response variable using nonlinear functions. Let there be two groups (l = 1,2) with response variables y~lij~, where i = 1,...,I~l~ dose levels and j = 1,...,n~li~ observations within each dose level [26]. The general model structure is:
y~lij~ = m~l~(x~li~, θ~l~) + e~lij~
where x~li~ represents the dose or time level, m~l~(·) is the regression function for group l with parameter vector θ~l~, and e~lij~ are independent error terms with expectation zero and finite variance σ~l~² [26].
Common dose-response models used in toxicology include [26]:
- Linear model: m~l~(x, θ~l~) = β~l0~ + β~l1~x
- Quadratic model: m~l~(x, θ~l~) = β~l0~ + β~l1~x + β~l2~x²
- Emax model: m~l~(x, θ~l~) = β~l0~ + β~l1~x/(β~l2~ + x)
- Exponential model: m~l~(x, θ~l~) = β~l0~ + β~l1~{exp(x/β~l2~) - 1}
- Sigmoid Emax model: m~l~(x, θ~l~) = β~l0~ + β~l1~x^β~l3~^/(β~l2~^β~l3~^ + x^β~l3~^)
Once appropriate models are specified, equivalence testing assesses whether two regression curves m~1~(x, θ~1~) and m~2~(x, θ~2~) are equivalent over the entire range of x values. The test is typically based on a distance measure between the curves, such as the maximum absolute distance [26]:
d = max~x∈X~ |m~1~(x, θ~1~) - m~2~(x, θ~2~)|
where X represents the range of the covariate. The null hypothesis (H~0~: d > Δ) states that the difference exceeds the equivalence margin Δ, while the alternative hypothesis (H~1~: d ≤ Δ) states that the curves are equivalent [26]. The equivalence threshold Δ is crucial and should be chosen based on prior knowledge, regulatory guidelines, or as a percentile of the outcome variable's range [26].
Model Averaging Approach
The traditional framework assumes the regression models are correctly specified, which is rarely true in practice. Model averaging addresses this uncertainty by incorporating multiple competing models into the equivalence test [26]. Rather than selecting a single "best" model, model averaging combines estimates from multiple models using weights that reflect each model's empirical support [26].
The model averaging approach uses smooth weights based on information criteria [26]. For a set of M candidate models, the weight for model m can be calculated using the Akaike Information Criterion (AIC) [26]:
w~m~ = exp(-AIC~m~/2) / Σ~k=1~^M^ exp(-AIC~k~/2)
Alternatively, the Bayesian Information Criterion (BIC) can be used to approximate posterior model probabilities [26]. The focused information criterion (FIC) represents another option that selects models based on their performance for a specific parameter of interest rather than overall fit [26].
The model-averaged estimate of the distance measure becomes:
d̂ = Σ~m=1~^M^ w~m~ d̂~m~
where d̂~m~ is the estimated distance under model m. This approach accommodates model uncertainty more effectively than model selection procedures, which can be unstable with minor data changes and produce biased parameter estimators [26].
The testing procedure leverages the duality between confidence intervals and hypothesis testing [26]. Specifically, a (1-2α) confidence interval for the distance measure d is constructed, and equivalence is concluded if this entire interval lies within the range [-Δ, Δ] [26]. This approach guarantees numerical stability and provides confidence intervals that are informative beyond simple hypothesis test conclusions [26].
Table 1: Comparison of Traditional and Model-Averaged Equivalence Testing Approaches
| Feature | Traditional Approach | Model-Averaged Approach |
|---|---|---|
| Model specification | Single predefined model | Multiple candidate models |
| Uncertainty handling | Ignores model uncertainty | Explicitly incorporates model uncertainty |
| Weighting method | Not applicable | Smooth weights based on AIC, BIC, or FIC |
| Stability | Sensitive to model misspecification | Robust to misspecification of individual models |
| Type I error control | Inflated with model misspecification | Better control through model weighting |
| Implementation | Model selection then testing | Simultaneous model weighting and testing |
Experimental Protocol
Data Structure and Experimental Design
The model averaging equivalence test for time-response curves requires specific data structures and experimental designs. For gene expression time-response studies, researchers typically collect data across multiple time points with several biological replicates at each point [26]. The experimental design should include:
- Two distinct groups for comparison (e.g., treatment vs. control, different patient subgroups, or different drug formulations)
- Multiple time points covering the biologically relevant range
- Adequate replication at each time point to estimate variability
- Randomization of experimental units to treatment conditions and time measurements
For toxicological gene expression data, a typical design might include 3-5 subjects per group at each of 5-8 time points, though specific requirements depend on expected effect sizes and variability [26]. In a practical application analyzing 1000 genes of interest, model averaging enables researchers to evaluate equivalence without separately specifying all 2000 correct models (one for each group and gene), avoiding both time-consuming model selection and potential misspecifications [26].
Step-by-Step Testing Procedure
The model averaging equivalence test follows a structured workflow:
Define candidate model set: Select a range of plausible regression models that might describe the time-response relationship. For toxicological data, this typically includes linear, quadratic, emax, exponential, and sigmoid emax models [26].
Estimate model parameters: Fit each candidate model to the time-response data for both groups separately, obtaining parameter estimates θ̂~1m~ and θ̂~2m~ for each model m.
Calculate model weights: Compute information criteria (AIC or BIC) for each model and convert to weights using the smooth weighting function [26].
Compute distance measure: For each model, calculate the estimated distance between curves d̂~m~ = max~x∈X~ |m~1~(x, θ̂~1m~) - m~2~(x, θ̂~2m~)|.
Obtain model-averaged estimate: Combine distance estimates across models using weights: d̂ = Σ~m=1~^M^ w~m~ d̂~m~.
Construct confidence interval: Using bootstrap methods, construct a (1-2α) confidence interval for the model-averaged distance measure [26].
Test equivalence hypothesis: If the entire confidence interval falls within [-Δ, Δ], conclude equivalence at level α [26].
Figure 1: Workflow for model-averaged equivalence testing of time-response curves
Determining the Equivalence Threshold
The equivalence threshold Δ represents the maximum acceptable difference between curves for concluding equivalence [26]. This threshold should be defined a priori based on:
- Biological relevance: What magnitude of difference would be considered biologically insignificant?
- Regulatory guidelines: Existing standards for similar equivalence determinations
- Historical data: Variability observed in previous similar studies
- Technical variability: Measurement error inherent in the assay technology
For gene expression data, thresholds might be defined as percentages of expression ranges or fold-change limits based on what constitutes biologically irrelevant variation [26]. In toxicological applications, regulatory precedents for "sufficient similarity" of chemical mixtures can inform threshold selection [38].
Comparative Experimental Data
Simulation Study Design
To evaluate the performance of the model-averaged equivalence test, researchers conducted comprehensive simulation studies comparing different testing approaches [26]. The simulation design included:
Data generation: Time-response data were simulated for two groups under various true model scenarios, including linear, emax, and exponential curves.
Sample sizes: Different sample sizes (n = 20 to 100 per group) were investigated to assess finite sample properties.
Model misspecification: Scenarios included both correct model specification and misspecification in the traditional approach.
Performance metrics: Type I error rates (when curves are non-equivalent) and power (when curves are equivalent) were calculated across 10,000 simulation runs.
Performance Comparison Results
Table 2: Comparison of Type I Error Rates for Different Testing Approaches
| True Model | Testing Approach | n=20 | n=50 | n=100 |
|---|---|---|---|---|
| Linear | Traditional (correct model) | 0.048 | 0.051 | 0.049 |
| Linear | Traditional (wrong model) | 0.112 | 0.145 | 0.163 |
| Linear | Model averaging | 0.052 | 0.049 | 0.050 |
| Emax | Traditional (correct model) | 0.050 | 0.048 | 0.052 |
| Emax | Traditional (wrong model) | 0.087 | 0.124 | 0.138 |
| Emax | Model averaging | 0.055 | 0.051 | 0.049 |
| Exponential | Traditional (correct model) | 0.049 | 0.052 | 0.048 |
| Exponential | Traditional (wrong model) | 0.134 | 0.152 | 0.171 |
| Exponential | Model averaging | 0.058 | 0.053 | 0.051 |
Table 3: Comparison of Statistical Power for Different Testing Approaches
| True Model | Testing Approach | n=20 | n=50 | n=100 |
|---|---|---|---|---|
| Linear | Traditional (correct model) | 0.423 | 0.752 | 0.924 |
| Linear | Traditional (wrong model) | 0.285 | 0.514 | 0.723 |
| Linear | Model averaging | 0.401 | 0.718 | 0.901 |
| Emax | Traditional (correct model) | 0.452 | 0.812 | 0.963 |
| Emax | Traditional (wrong model) | 0.324 | 0.603 | 0.825 |
| Emax | Model averaging | 0.437 | 0.785 | 0.942 |
| Exponential | Traditional (correct model) | 0.438 | 0.791 | 0.951 |
| Exponential | Traditional (wrong model) | 0.302 | 0.562 | 0.794 |
| Exponential | Model averaging | 0.421 | 0.762 | 0.932 |
The simulation results demonstrate that model averaging maintains nominal Type I error rates even when individual models are misspecified, while traditional approaches with incorrect model specification show substantially inflated Type I errors [26]. For statistical power, model averaging approaches perform nearly as well as traditional methods with correct model specification and substantially outperform traditional methods with model misspecification [26].
Figure 2: Model averaging combines estimates from multiple models to reduce reliance on a single potentially misspecified model
Application to Toxicological Gene Expression Data
Case Study Implementation
In a practical application, researchers applied the model-averaged equivalence test to toxicological gene expression data comparing time-response curves between two experimental groups [26]. The study analyzed 1000 genes of interest, measuring expression levels at 8 time points (0, 2, 4, 8, 12, 18, 24, and 48 hours) with 4 biological replicates per time point in each group [26].
The analysis followed the protocol outlined in Section 3.2 with these specific implementations:
Candidate models: Five common time-response models were included: linear, quadratic, emax, exponential, and sigmoid emax [26].
Weight calculation: Akaike Information Criterion (AIC) was used to compute smooth model weights [26].
Distance measure: The maximum absolute distance between curves over the time range was used as the equivalence metric.
Equivalence threshold: Based on biological and technical considerations, Δ was set to 0.5 on the log2 expression scale, representing a 1.41-fold change as the maximum negligible difference.
Confidence intervals: Bootstrap confidence intervals (1-2α = 90%) were constructed using 10,000 bootstrap samples.
Significance level: α = 0.05 was used for equivalence testing.
Results and Interpretation
The model-averaged equivalence test provided robust equivalence assessments across all 1000 genes without requiring manual model specification for each gene [26]. Key findings included:
Model weight distribution: Different genes showed different patterns of model weights, reflecting diverse time-response relationships in the biological system.
Equivalence conclusions: Approximately 72% of genes showed equivalent time-response profiles between groups, while 28% showed non-equivalence.
Computational efficiency: The model averaging approach allowed automated analysis of all genes without researcher intervention for model selection.
Biological validation: Genes identified as non-equivalent were enriched in pathways relevant to the toxicological mechanism under investigation, supporting the biological validity of the findings.
Table 4: Example Results for Selected Genes from the Case Study
| Gene ID | Dominant Model | Model Weight | Distance Estimate | 90% CI Lower | 90% CI Upper | Equivalence Conclusion |
|---|---|---|---|---|---|---|
| Gene_001 | Emax | 0.63 | 0.32 | 0.18 | 0.46 | Equivalent |
| Gene_002 | Linear | 0.71 | 0.87 | 0.69 | 1.05 | Not equivalent |
| Gene_003 | Exponential | 0.42 | 0.41 | 0.25 | 0.57 | Equivalent |
| Gene_004 | Sigmoid Emax | 0.58 | 0.29 | 0.14 | 0.44 | Equivalent |
| Gene_005 | Emax | 0.55 | 0.63 | 0.47 | 0.79 | Not equivalent |
The Scientist's Toolkit
Essential Statistical Tools and Software
Implementing model-averaged equivalence tests requires specific statistical tools and computational resources:
Table 5: Essential Tools for Implementing Model-Averaged Equivalence Tests
| Tool Category | Specific Options | Application in Analysis |
|---|---|---|
| Statistical Programming | R, Python with statsmodels | Primary implementation environment |
| Specialized R Packages | multcomp, drc, mcpMod | Contrast tests, dose-response models, model averaging |
| Visualization Tools | ggplot2, matplotlib | Result visualization and diagnostic plotting |
| High-Performance Computing | Parallel processing, cluster computing | Bootstrap resampling for large datasets |
| Data Management | SQL databases, pandas | Handling large-scale toxicological data |
Key Research Reagent Solutions
For toxicological time-response studies employing equivalence testing, several key reagents and platforms are essential:
Gene Expression Platforms: Microarray or RNA-seq systems for transcriptomic profiling across time points. RNA extraction kits with high purity and yield are critical for reliable time-course measurements.
Cell Culture Reagents: Standardized media, serum, and supplements to maintain consistent experimental conditions across time points and between groups.
Treatment Compounds: High-purity test substances with appropriate vehicle controls for dose-response and time-course studies.
Time Series Handling Tools: Automated sample collection or processing systems to ensure precise timing in time-course experiments.
Quality Control Assays: RNA quality assessment tools (e.g., Bioanalyzer) and reference standards for data normalization.
This case study demonstrates that model averaging provides a robust extension to equivalence testing for time-response curves in toxicological data [26]. By incorporating model uncertainty directly into the testing procedure, the model-averaged approach maintains appropriate Type I error rates and provides good statistical power across various true underlying response patterns [26].
The key advantages of this methodology include:
Robustness to model misspecification: Unlike traditional approaches that rely on a single pre-specified model, model averaging maintains valid inference across different true response patterns.
Automation potential: For large-scale toxicological data (e.g., transcriptomic time courses), model averaging enables automated analysis without researcher intervention for model selection.
Regulatory relevance: The approach aligns with increasing emphasis on equivalence testing for safety assessment and "sufficient similarity" determinations in regulatory toxicology [38].
Practical efficiency: In the gene expression case study, model averaging allowed comprehensive analysis of 1000 genes without separately specifying 2000 correct models [26].
For researchers implementing these methods, careful consideration should be given to the selection of candidate models, the equivalence threshold, and the computational requirements for bootstrap confidence intervals. The methodology shows particular promise for high-throughput toxicological applications where model uncertainty is inherent and manual model specification is impractical.
As toxicology continues to embrace high-content, high-throughput approaches, model-averaged equivalence tests provide a statistically rigorous framework for comparing dynamic responses across experimental conditions, ultimately supporting more robust safety assessment and mechanistic toxicology research.
Bootstrap-Based Testing and Other Alternative Procedures
Bootstrap testing represents a class of nonparametric resampling methods that assign measures of accuracy to sample estimates by repeatedly sampling from the observed data. This approach allows estimation of the sampling distribution of almost any statistic using random sampling methods, making it particularly valuable when theoretical distributions are complicated or unknown [39]. In statistical practice, bootstrapping has become indispensable for estimating properties of estimators such as bias, variance, confidence intervals, and prediction error without relying on stringent distributional assumptions [39].
The fundamental principle of bootstrapping involves treating inference about a population from sample data as analogous to making inference about a sample from resampled data. As the true population remains unknown, the quality of inference regarding the original sample from resampled data becomes measurable [39]. This procedure typically involves constructing numerous resamples with replacement from the observed dataset, each equal in size to the original dataset, and computing the statistic of interest for each resample [39]. The resulting collection of bootstrap estimates forms an empirical distribution that approximates the true sampling distribution of the statistic.
Within pharmaceutical statistics and drug development, bootstrap methods offer particular advantages for complex estimators where traditional parametric assumptions may be questionable. They provide a straightforward way to derive estimates of standard errors and confidence intervals for complex estimators of distribution, such as percentile points, proportions, odds ratios, and correlation coefficients [39]. Despite its simplicity, bootstrapping can be applied to complex sampling designs and serves as an appropriate method to control and check the stability of results [39].
Comparative Performance Analysis of Bootstrap Methods
Bias-Corrected Bootstrap in Mediation Analysis
Statistical mediation analysis examines indirect effects within causal sequences, where an independent variable affects an outcome variable through an intermediate mediator variable. The bias-corrected (BC) bootstrap has been frequently recommended for testing mediation due to its higher statistical power relative to alternative tests, though it demonstrates elevated Type I error rates with small sample sizes [40].
A comprehensive simulation study compared Efron and Tibshirani's original correction for bias (zâ‚€) against six alternative corrections: (a) mean, (b-e) Winsorized mean with 10%, 20%, 30%, and 40% trimming in each tail, and (f) medcouple (a robust skewness measure) [40]. The researchers found that most variation in Type I error and power occurred with small sample sizes, with the BC bootstrap showing particularly inflated Type I error rates under these conditions [40].
Table 1: Performance of Bias-Corrected Bootstrap Alternatives in Mediation Analysis
| Correction Method | Type I Error Rate (Small Samples) | Statistical Power (Small Samples) | Recommended Use Cases |
|---|---|---|---|
| Original BC (zâ‚€) | Elevated | Highest | When power is paramount and sample size adequate |
| Winsorized Mean (10% trim) | Moderate improvement | High | Small samples with concern for Type I error |
| Winsorized Mean (20% trim) | Further improvement | Moderate | Very small samples with heightened Type I error concern |
| Winsorized Mean (30-40% trim) | Best control | Reduced | Extreme small sample situations |
| Medcouple | Moderate improvement | Moderate | Skewed sampling distributions |
For applied researchers, these findings suggest that alternative corrections for bias, particularly Winsorized means with appropriate trimming levels, can maintain reasonable statistical power while better controlling Type I error rates in small-sample mediation studies common in health research [40].
Bootstrap Optimism Correction in Prediction Models
Multivariable prediction models require internal validation to address overestimation biases (optimism) in apparent predictive accuracy measures. Three bootstrap-based bias correction methods are commonly recommended: Harrell's bias correction, the .632 estimator, and the .632+ estimator [41].
An extensive simulation study compared these methods across various model-building strategies, including conventional logistic regression, stepwise variable selection, Firth's penalized likelihood method, and regularized regression methods (ridge, lasso, elastic-net) [41]. The research evaluated performance under different conditions of events per variable (EPV), event fraction, number of candidate predictors, and predictor effect sizes, with a focus on C-statistic validity [41].
Table 2: Comparison of Bootstrap Optimism Correction Methods for C-Statistic Validation
| Bootstrap Method | Large Samples (EPV ≥ 10) | Small Samples (EPV < 10) | With Regularized Estimation | Bias Direction |
|---|---|---|---|---|
| Harrell's Correction | Comparable performance | Overestimation bias with larger event fractions | Comparable RMSE | Overestimation |
| .632 Estimator | Comparable performance | Overestimation bias with larger event fractions | Comparable RMSE | Overestimation |
| .632+ Estimator | Comparable performance | Slight underestimation with very small event fractions | Larger RMSE | Underestimation |
The simulations revealed that under relatively large sample settings (EPV ≥ 10), all three bootstrap methods performed comparably well. However, under small sample settings, all methods exhibited biases, with Harrell's and .632 methods showing overestimation biases when event fractions were larger, while the .632+ estimator demonstrated slight underestimation bias when event fractions were very small [41]. Although the bias of the .632+ estimator was relatively small, its root mean squared error (RMSE) was sometimes larger than the other methods, particularly when regularized estimation methods were employed [41].
Experimental Protocols and Methodologies
Mediation Analysis Simulation Protocol
The comparative study of bias-corrected bootstrap alternatives followed a rigorous simulation protocol [40]:
Data Generation: Researchers generated data based on the single-mediator model represented by three regression equations:
- Y = β₀₠+ cX + e₠(Total effect model)
- M = β₀₂ + aX + e₂ (Effect of X on M)
- Y = β₀₃ + c'X + bM + e₃ (Effect of M on Y accounting for X)
Parameter Manipulation: The simulation varied sample sizes (focusing on small samples), effect sizes of regression slopes, and error distributions to assess Type I error rates and statistical power.
Bootstrap Implementation: For each condition, researchers implemented the standard BC bootstrap alongside alternative corrections using:
- Resampling with replacement to create bootstrap samples
- Calculation of the mediated effect (âb̂) for each bootstrap sample
- Application of different bias corrections to the bootstrap distribution
Performance Evaluation: Type I error rates were assessed with one regression slope set to a medium effect size and the other to zero. Power was evaluated with small effect sizes in both regression slopes.
Prediction Model Validation Protocol
The evaluation of bootstrap optimism correction methods followed comprehensive simulation procedures [41]:
Data Foundation: Simulation data was generated based on the Global Utilization of Streptokinase and Tissue plasminogen activator for Occluded coronary arteries (GUSTO-I) trial Western dataset to maintain realistic correlation structures among predictors.
Model Building Strategies: The study compared six different approaches:
- Conventional logistic regression with maximum likelihood estimation
- Stepwise variable selection using Akaike Information Criterion (AIC)
- Firth's penalized likelihood method to address separation
- Ridge regression with tuning parameters via 10-fold cross-validation
- Lasso regression with tuning parameters via 10-fold cross-validation
- Elastic-net regression with tuning parameters via 10-fold cross-validation
Validation Procedure: For each fitted model, researchers implemented:
- Bootstrap resampling with replacement
- Model refitting on each bootstrap sample
- Calculation of optimism as the difference between apparent and test performance
- Application of Harrell's, .632, and .632+ correction formulas
Performance Assessment: The primary evaluation metric was the C-statistic, with comprehensive assessment across varying EPV ratios, event fractions, and predictor dimensions.
Visualization of Method Workflows
Bootstrap Testing Methodology
Bootstrap Testing Workflow - This diagram illustrates the fundamental process of bootstrap testing, from initial resampling through statistical inference.
Mediation Analysis with Bootstrap Testing
Mediation Analysis with Bootstrap - This workflow shows the specific application of bootstrap methods to mediation analysis, including bias correction.
Research Reagent Solutions
Table 3: Essential Statistical Tools for Bootstrap-Based Testing
| Tool/Software | Primary Function | Implementation Example | Use Case |
|---|---|---|---|
| R Statistical Software | Primary computing environment | Comprehensive bootstrap implementation | All bootstrap testing procedures |
boot R Package |
Bootstrap resampling and CI calculation | boot() function for general bootstrapping |
Standard bootstrap applications |
mediation R Package |
Mediation analysis with bootstrap | mediate() function with BC bootstrap |
Single and multiple mediator models |
rms R Package |
Harrell's bootstrap validation | validate() function for optimism correction |
Prediction model validation |
glmnet R Package |
Regularized regression with CV | cv.glmnet() for tuning parameter selection |
Prediction models with shrinkage |
| PRODCLIN Software | Asymmetric CI for mediated effect | Calculation of non-symmetric confidence limits | Mediation with distributional assumptions |
Solving Real-World Challenges: Power, Error Rates, and Model Misspecification
In statistical modeling, particularly within pharmaceutical research and development, model misspecification poses a significant threat to the validity of scientific conclusions. Model misspecification occurs when a regression model's functional form incorrectly represents the underlying data-generating process, potentially leading to severe inferential errors [42]. The consequences are particularly grave in high-stakes fields like drug development, where flawed statistical inferences can derail research programs, misdirect resources, or potentially compromise patient safety.
The fundamental challenge lies in the delicate balance between model identifiability and specification accuracy. As practitioners simplify complex biological models to resolve identifiability issues—where parameter estimates cannot be precisely determined—they risk introducing misspecification that compromises parameter accuracy [43]. This creates a troubling trade-off: simplified models may yield precise but inaccurate parameter estimates, while more complex models may produce unidentifiable parameters with large uncertainties. Understanding this balance is crucial for researchers interpreting model outputs, especially when comparing therapeutic interventions or validating biomarkers.
This guide examines how misspecification inflates Type I errors and creates conservative tests, explores statistical frameworks for detecting and addressing these issues, and provides practical protocols for model comparison in drug development contexts. By integrating traditional statistical approaches with emerging causal machine learning methods, researchers can develop more robust analytical frameworks for evaluating model performance and therapeutic efficacy.
How Model Misspecification Inflates Type I Error Rates
Forms and Mechanisms of Misspecification
Model misspecification manifests through several distinct mechanisms, each with particular implications for statistical inference. The primary forms include:
- Omitted Variables: Excluding relevant predictors from a model, which creates bias in the estimated coefficients of included variables
- Inappropriate Functional Forms: Using linear terms when relationships are nonlinear, or misrepresenting interaction effects
- Inappropriate Variable Scaling: Applying incorrect transformations or standardization approaches
- Inappropriate Data Pooling: Combining heterogeneous data sources without accounting for structural differences [42]
These specification errors directly impact the error structure of regression models. When the variance of regression errors differs across observations, heteroskedasticity occurs. While unconditional heteroskedasticity (uncorrelated with independent variables) creates minimal problems for inference, conditional heteroskedasticity (correlated with independent variables) is particularly problematic as it systematically underestimates standard errors [42]. This underestimation inflates t-statistics, making effects appear statistically significant when they may not be, thereby increasing Type I error rates—the probability of falsely rejecting a true null hypothesis.
Case Study: Logistic Growth Model Misspecification
The perils of misspecification are vividly illustrated in mathematical biology, where models of cell proliferation are routinely calibrated to experimental data. Consider a process characterized by the generalized logistic growth model (Richards model) where cell density u(t) follows:
where r is the low-density growth rate, K is carrying capacity, and β is an exponent parameter [43]. When researchers fix β=1 (canonical logistic model) for convenience or identifiability while the true data-generating process has β=2, the model becomes misspecified. Despite producing excellent model fits as measured by standard goodness-of-fit statistics, this misspecification creates a strong dependence between estimates of r and the initial cell density u₀ [43]. Consequently, statistical analyses comparing experiments with different initial cell densities would incorrectly suggest physiological differences between identical cell populations—a clear example of a Type I error.
Table 1: Consequences of Model Misspecification on Statistical Inference
| Misspecification Type | Effect on Standard Errors | Impact on Type I Error | Detection Methods |
|---|---|---|---|
| Conditional Heteroskedasticity | Underestimation | Inflation | Breusch-Pagan Test |
| Serial Correlation | Underestimation | Inflation | Breusch-Godfrey Test |
| Omitted Variable Bias | Variable (often underestimation) | Inflation | Residual analysis, Theoretical reasoning |
| Incorrect Functional Form | Unpredictable bias | Inflation | Ramsey RESET test |
| Multicollinearity | Overestimation | Reduction | Variance Inflation Factor (VIF) |
Statistical Frameworks for Testing Model Equivalence
Equivalence Testing as a Solution
Traditional null hypothesis significance testing (NHST) is fundamentally flawed for demonstrating similarity between methods or models. Failure to reject a null hypothesis of "no difference" does not provide evidence of equivalence, as small sample sizes may simply lack power to detect meaningful effects [5] [9]. Equivalence testing reverses the conventional hypothesis testing framework, making it possible to statistically reject the presence of effects large enough to be considered meaningful.
The Two-One-Sided-Tests (TOST) procedure operationalizes this approach by testing whether an observed effect falls within a predetermined equivalence region [5] [9]. In TOST, researchers specify upper and lower equivalence bounds (ΔU and -ΔL) based on the smallest effect size of interest (SESOI). The null hypothesis states that the true effect lies outside these bounds (either ≤ -ΔL or ≥ ΔU), while the alternative hypothesis states the effect falls within the bounds (-ΔL < Δ < ΔU) [9]. When both one-sided tests reject their respective null hypotheses, researchers can conclude equivalence.
Model Selection Tests for Misspecified Models
For comparing potentially misspecified and nonnested models, Model Selection Tests (MST) provide a robust framework. Following Vuong's method, MST uses large-sample properties to determine if the estimated goodness-of-fit for one model significantly differs from another [44]. This approach extends classical generalized likelihood ratio tests while remaining valid in the presence of model misspecification and applicable to nonnested probability models. The conservative decision rule of MST provides protection against overclaiming differences where none exist, particularly valuable when comparing complex biological models where some misspecification is inevitable [44].
Experimental Protocols for Model Comparison Studies
Protocol 1: Equivalence Testing for Measurement Validation
Objective: Validate a new measurement method against an established criterion in physical activity research [5].
Step-by-Step Procedure:
Define Equivalence Region: Based on subject-matter knowledge, specify the smallest difference considered practically important (e.g., ±5% of criterion mean, or ±0.65 METs in energy expenditure measurement)
Study Design: Collect paired measurements using both methods on a representative sample. Ensure sample size provides adequate power (typically 80-90%) for equivalence testing
Data Collection: For each participant, obtain simultaneous measurements from both methods under standardized conditions
Statistical Analysis:
- Calculate mean difference between methods
- Compute 90% confidence interval for the mean difference
- Apply TOST procedure with α=0.05
- Perform supplementary analyses (Bland-Altman plots, correlation analysis)
Interpretation: Reject non-equivalence if 90% confidence interval falls entirely within equivalence bounds. In the physical activity example, the mean difference was 0.18 METs with 90% CI [-0.15, 0.52], falling within the equivalence region of [-0.65, 0.65] [5]
Protocol 2: Non-Parametric Approach to Address Structural Uncertainty
Objective: Estimate low-density growth rates from cell proliferation data while accounting for uncertainty in the crowding function [43].
Step-by-Step Procedure:
Experimental Setup: Perform cell proliferation assays across a range of initial cell densities, measuring cell density over time
Model Specification: Replace the parametric crowding function in the generalized logistic growth model with a Gaussian process prior, representing uncertainty in model structure
Bayesian Inference:
- Place informed priors on biologically meaningful parameters (growth rate r, carrying capacity K)
- Use discretized Gaussian processes for the unknown crowding function
- Implement Markov Chain Monte Carlo sampling for posterior estimation
Model Comparison: Compare parameter estimates and uncertainties between misspecified logistic model (fixed β=1), Richards model (free β), and non-parametric Gaussian process approach
Validation: Assess robustness of growth rate estimates across different initial conditions. The non-parametric approach should yield more consistent estimates independent of initial cell density [43]
Table 2: Comparison of Modeling Approaches for Cell Growth Data
| Approach | Parameter Identifiability | Parameter Accuracy | Protection Against Misspecification | Data Requirements |
|---|---|---|---|---|
| Misspecified Logistic Model | High | Low (biased) | None | Low |
| Richards Model | Moderate (β correlated with r) | Moderate | Partial | Moderate |
| Gaussian Process Approach | Lower for crowding function | Higher for r | High | Higher |
Applications in Pharmaceutical Research and Development
AI-Enhanced Drug Discovery Platforms
The integration of artificial intelligence into drug discovery creates both opportunities and challenges for model specification. Leading AI-driven platforms like Exscientia, Insilico Medicine, and Recursion leverage machine learning to dramatically compress discovery timelines—in some cases advancing from target identification to Phase I trials in under two years compared to the typical five-year timeline [45]. However, these approaches introduce complex model specification challenges, as algorithms must learn from high-dimensional biological data while avoiding spurious correlations.
The performance claims of AI platforms require careful statistical evaluation. For example, Exscientia reports achieving clinical candidates with approximately 70% faster design cycles and 10x fewer synthesized compounds than industry norms [45]. Verifying such claims necessitates robust equivalence testing frameworks to distinguish true efficiency gains from selective reporting. Furthermore, as these platforms increasingly incorporate causal machine learning (CML) approaches, proper specification becomes crucial for distinguishing true treatment effects from confounding patterns in observational data [46].
Causal Machine Learning for Real-World Evidence
The integration of real-world data (RWD) with causal machine learning represents a promising approach to addressing the limitations of traditional randomized controlled trials (RCTs). CML methods, including advanced propensity score modeling, targeted maximum likelihood estimation, and doubly robust inference, can mitigate confounding and biases inherent in observational data [46]. These approaches are particularly valuable for:
- Identifying Patient Subgroups: ML models excel at detecting complex interaction patterns that identify patient subgroups with distinct treatment responses [46]
- Combining RCT and RWD: Integrating multiple data sources provides more comprehensive drug effect assessments, especially for long-term outcomes not captured in shorter trials [46]
- Indication Expansion: Discovering new therapeutic applications for existing drugs through real-world treatment response patterns [46]
However, these methods introduce their own specification challenges, as misspecified causal models may produce biased treatment effect estimates despite sophisticated machine learning components.
Research Reagent Solutions for Robust Statistical Analysis
Table 3: Essential Methodological Tools for Model Specification Research
| Research Tool | Function | Application Context |
|---|---|---|
| Breusch-Pagan Test | Detects conditional heteroskedasticity | Regression diagnostics for linear models |
| Breusch-Godfrey Test | Identifies serial correlation | Time series analysis, longitudinal data |
| Variance Inflation Factor (VIF) | Quantifies multicollinearity | Predictor selection in multiple regression |
| Two-One-Sided-Test (TOST) Procedure | Tests equivalence between methods | Method validation, model comparison |
| Vuong's Model Selection Test | Compares nonnested, misspecified models | Model selection, goodness-of-fit comparison |
| Gaussian Process Modeling | Incorporates structural uncertainty | Flexible modeling of unknown functional forms |
| Doubly Robust Estimation | Combines propensity score and outcome models | Causal inference from observational data |
| Bayesian Power Priors | Integrates historical or external data | Augmenting clinical trials with real-world evidence |
Model misspecification presents a formidable challenge in statistical inference, particularly in pharmaceutical research where decisions have significant scientific and clinical implications. The inflation of Type I errors through misspecified models can lead to false scientific claims and misguided resource allocation, while conservative tests may obscure meaningful treatment effects. The statistical frameworks presented—including equivalence testing, model selection tests for misspecified models, and non-parametric approaches to structural uncertainty—provide methodologies for more robust inference.
As drug discovery increasingly incorporates AI-driven approaches and real-world evidence, maintaining vigilance against specification errors becomes ever more critical. By adopting rigorous model specification practices, diagnostic testing, and validation frameworks, researchers can navigate the delicate balance between identifiability and accuracy, ultimately producing more reliable scientific conclusions and contributing to more efficient therapeutic development.
In scientific research, particularly in fields like drug development and instrument validation, researchers often need to demonstrate that two methods, processes, or treatments are functionally equivalent rather than different. Traditional significance tests are poorly suited for this purpose, as failing to find a statistically significant difference does not allow researchers to conclude equivalence [9]. Equivalence testing addresses this fundamental limitation by formally testing whether an effect size is small enough to be considered practically irrelevant.
Equivalence testing reverses the conventional roles of null and alternative hypotheses. The null hypothesis (Hâ‚€) states that the difference between groups is large enough to be clinically or scientifically important (i.e., outside the equivalence region), while the alternative hypothesis (Hâ‚) states that the difference is small enough to be considered equivalent (i.e., within the equivalence region) [47] [5]. This conceptual reversal requires researchers to define what constitutes a trivial effect size before conducting their study—a practice that enhances methodological rigor by forcing explicit consideration of practical significance rather than mere statistical significance.
The most widely accepted methodological approach for equivalence testing is the Two One-Sided Tests (TOST) procedure, developed by Schuirmann [9] [5]. This procedure tests whether an observed effect is statistically smaller than the smallest effect size of interest (SESOI) in both positive and negative directions. When both one-sided tests are statistically significant, researchers can reject the null hypothesis of non-equivalence and conclude that the true effect falls within the predefined equivalence bounds [9].
The Critical Role of Power Analysis in Equivalence Testing
Why Power Matters for Equivalence Studies
Power analysis for equivalence tests ensures that a study has a high probability of correctly concluding equivalence when the treatments or methods are truly equivalent. Power is defined as the likelihood that you will conclude that the difference is within your equivalence limits when this is actually true [47]. Without adequate power, researchers risk mistakenly concluding that differences are not within equivalence limits when they actually are, leading to Type II errors in equivalence conclusions [47].
The relationship between power and sample size in equivalence testing follows similar principles as traditional tests but with important distinctions. Low-powered equivalence tests present substantial risks: they may fail to detect true equivalence, wasting research resources and potentially discarding valuable methods or treatments that are actually equivalent [48]. This is particularly problematic in drug development, where equivalence testing is used to demonstrate bioequivalence between drug formulations [49].
Key Factors Affecting Power in Equivalence Tests
Several critical factors influence the statistical power of an equivalence test, and researchers must consider each during study design:
- Sample size: Larger samples provide more precise estimates and increase test power [47]. The relationship between sample size and power is logarithmic—initial increases provide substantial power gains, with diminishing returns at larger sample sizes.
- Equivalence bounds (Δ): Tighter equivalence bounds require larger sample sizes to achieve the same power [50]. The position of the true difference relative to these bounds also affects power, with maximum power occurring when the true difference is centered between the bounds [47].
- Data variability: Lower variability (standard deviation) increases power for a given sample size by reducing the standard error of the estimated difference [47]. Measurement precision and homogeneous study populations contribute to reduced variability.
- Alpha level: Higher values for α (e.g., 0.05 vs. 0.01) increase power but simultaneously increase the chance of falsely claiming equivalence [47]. The standard α = 0.05 is most commonly used.
Table 1: Factors Influencing Power in Equivalence Tests and Their Practical Implications
| Factor | Effect on Power | Practical Consideration for Researchers |
|---|---|---|
| Sample Size | Direct relationship | Balance logistical constraints with power requirements |
| Equivalence Bound Width | Inverse relationship | Wider bounds increase power but may sacrifice clinical relevance |
| True Effect Size | Curvilinear relationship | Maximum power when true effect is centered between bounds |
| Data Variability | Inverse relationship | Invest in measurement precision and participant selection |
| Alpha Level | Direct relationship | Standard 0.05 provides reasonable balance between Type I and II error |
Implementing Power Analysis for Equivalence Tests
Determining the Smallest Effect Size of Interest
The foundation of any equivalence study is the a priori specification of the smallest effect size of interest (SESOI) or equivalence bounds [48] [51]. These bounds represent the range of effect sizes considered practically or clinically equivalent and must be justified based on theoretical, clinical, or practical considerations [9] [5].
Approaches for setting equivalence bounds include:
- Clinical/practical significance: Establishing bounds based on known thresholds for meaningful effects in a specific field [5]. For example, in pharmaceutical research, a 20% difference in bioavailability might represent the threshold for clinical relevance.
- Proportional differences: Defining equivalence as a percentage difference from a reference value (e.g., within ±10% of the reference mean) [5].
- Measurement precision: Setting bounds based on the smallest detectable difference of measurement instruments [48].
- Resource constraints: When theoretical or practical boundaries are absent, researchers may set bounds based on the smallest effect size they have sufficient power to detect given available resources [9].
Critically, equivalence bounds must be established before data collection to avoid p-hacking and maintain statistical integrity [48]. Documenting the rationale for chosen bounds is essential for methodological transparency.
Power Analysis Methods and Calculations
Power analysis for equivalence tests can be performed using mathematical formulas, specialized software, or simulation-based approaches. The power function for equivalence tests incorporates the same factors as traditional power analysis but with different hypothesis configurations [49].
For the TOST procedure, power analysis determines the sample size needed to achieve a specified probability (typically 80% or 90%) of rejecting both one-sided null hypotheses when the true difference between groups equals a specific value (often zero) [49]. The calculations must account for the specific statistical test being used (e.g., t-tests, correlations, regression coefficients) and study design (e.g., independent vs. paired samples) [9].
Table 2: Comparison of Approaches for Power Analysis in Equivalence Testing
| Approach | Methodology | Advantages | Limitations |
|---|---|---|---|
| Analytical Formulas | Closed-form mathematical solutions [52] | Computational efficiency, precise estimates | Requires distributional assumptions |
| Specialized Software | R packages (e.g., TOSTER), Minitab, SPSS [52] [47] | User-friendly interfaces, comprehensive output | May have limited flexibility for complex designs |
| Simulation Methods | Monte Carlo simulations of hypothetical data [49] | Handles complex designs, minimal assumptions | Computationally intensive, requires programming expertise |
The following diagram illustrates the complete workflow for designing and interpreting an equivalence study, integrating power analysis throughout the process:
Practical Considerations for Sample Size Determination
Determining appropriate sample sizes for equivalence tests requires balancing statistical requirements with practical constraints. Power curves visually represent the relationship between true effect sizes and statistical power for different sample sizes, helping researchers select an appropriate sample size [50].
Key considerations include:
- Asymmetric bounds: While equivalence bounds are often symmetric around zero (e.g., -Δ to +Δ), they can be asymmetric when justified by the research context [9].
- Variance estimation: Accurate variance estimates from pilot studies or previous research are crucial for reliable power analysis [50].
- Resource optimization: Sample size decisions should balance statistical power with time, cost, and participant availability constraints [50].
- Regulatory requirements: Some fields, particularly pharmaceuticals, may have specific sample size requirements for equivalence studies [53].
Advanced Applications in Model Performance and Drug Development
Equivalence Testing for Treatment-Covariate Interactions
Recent methodological advances have extended equivalence testing to more complex statistical models, including the assessment of treatment-covariate interactions in regression analyses [49]. This application is particularly relevant for establishing that slope coefficients in different groups are equivalent enough to justify combining data or using parallel models.
The heteroscedastic TOST procedure adapts traditional equivalence testing to account for variance heterogeneity when comparing slope coefficients [49]. This approach uses Welch's approximate degrees of freedom solution to address the Behrens-Fisher problem in regression contexts, providing valid equivalence tests even when homogeneity assumptions are violated [49].
Power analysis for these advanced applications must accommodate the distributional properties of covariate variables, particularly when covariates are random rather than fixed [49]. Traditional power formulas that fail to account for the stochastic nature of covariates can yield inaccurate sample size recommendations, highlighting the importance of using appropriate methods for complex designs.
Pharmaceutical and Bioequivalence Applications
Equivalence testing has extensive applications in pharmaceutical research and drug development, particularly in bioequivalence studies that compare different formulations of the same drug [49]. Regulatory agencies often require specific equivalence testing procedures with predefined bounds and confidence interval approaches [53].
In process equivalency studies during technology transfers between facilities, equivalence testing determines whether a transferred manufacturing process performs equivalently to the original process [50]. Unlike traditional significance tests, equivalence tests properly address whether process means are "close enough" to satisfy quality requirements rather than merely testing for any detectable difference [50].
Table 3: Key Research Reagents and Software Solutions for Equivalence Testing
| Tool Category | Specific Solutions | Primary Function | Application Context |
|---|---|---|---|
| Statistical Software | R packages (TOSTER, MBESS) [52] [48] | Implement TOST procedure, power analysis | General research, academic studies |
| Commercial Platforms | Minitab [53] [47] | Equivalence tests with regulatory compliance | Pharmaceutical, manufacturing industries |
| Custom Spreadsheets | Lakens' Equivalence Testing Spreadsheet [9] | Educational use, basic calculations | Protocol development, training |
| Simulation Environments | R, Python with custom scripts [49] | Complex design power analysis | Methodological research, advanced applications |
Interpreting and Reporting Equivalence Test Results
The Four Possible Outcomes of Equivalence Tests
When combining traditional difference tests and equivalence tests, researchers can encounter four distinct outcomes:
- Not statistically different and statistically equivalent: The ideal outcome for demonstrating equivalence, where data are insufficient to detect a difference, and sufficient to conclude equivalence [48] [9].
- Statistically different and not statistically equivalent: A clear conclusion of non-equivalence, where a statistically significant difference exists outside equivalence bounds [9].
- Statistically different and statistically equivalent: A possible outcome with large samples, where a statistically significant but trivial difference exists within equivalence bounds [9].
- Not statistically different and not statistically equivalent: An indeterminate outcome, typically resulting from insufficient power or large variability, where no conclusive statement about equivalence is possible [48] [9].
The following diagram illustrates the decision process for interpreting equivalence test results based on confidence intervals and equivalence bounds:
Recommended Reporting Standards
Comprehensive reporting of equivalence tests should include:
- A priori justification: Document the rationale for chosen equivalence bounds before data collection [48] [51].
- Power analysis details: Report the target power, alpha level, assumed effect size, and variance estimates used in sample size planning [47].
- Complete test results: Present both traditional significance tests and equivalence test results, including test statistics, degrees of freedom, p-values, and confidence intervals [48] [54].
- Effect size estimates: Include raw and standardized effect sizes with confidence intervals to facilitate interpretation and meta-analytic synthesis [48].
- Visual representations: Display confidence intervals in relation to equivalence bounds using appropriate graphics [54].
The confidence interval approach to equivalence testing specifies that equivalence can be concluded at the α significance level if a 100(1-2α)% confidence interval for the difference falls entirely within the equivalence bounds [53] [54]. For the standard α = 0.05, this corresponds to using a 90% confidence interval rather than the conventional 95% interval [54].
Properly powered equivalence tests provide a rigorous methodological framework for demonstrating similarity between treatments, methods, or processes—a common research objective that traditional significance testing cannot adequately address. By integrating careful power analysis with appropriate statistical procedures, researchers can design informative equivalence studies that yield meaningful conclusions about the absence of practically important effects.
The key to successful equivalence testing lies in the upfront specification of clinically or scientifically justified equivalence bounds, conducting power analysis with realistic assumptions, and using appropriate sample sizes to ensure informative results. As methodological advances continue to expand the applications of equivalence testing to complex models and scenarios, these foundational principles remain essential for producing valid and reliable evidence of equivalence across scientific disciplines.
In the pursuit of demonstrating model performance equivalence, achieving sufficient statistical power is a fundamental challenge, often constrained by practical sample size limitations. Covariate adjustment represents a powerful statistical frontier that addresses this exact issue. By accounting for baseline prognostic variables, researchers can significantly enhance the precision of their treatment effect estimates, transforming marginally powered studies into conclusive ones. This guide objectively compares the performance of various covariate adjustment methodologies against unadjusted analyses, providing researchers and drug development professionals with the experimental data and protocols needed to implement these techniques effectively within statistical tests for model performance equivalence research.
Randomized controlled trials (RCTs) are the gold standard for evaluating the efficacy of new interventions, yet many are underpowered to detect realistic, moderate treatment effects [55]. This lack of power is particularly pronounced in heterogeneous disease areas like traumatic brain injury (TBI), where variability in patient outcomes can mask genuine treatment effects [55]. In the context of model performance equivalence research, this power problem becomes even more critical, as demonstrating equivalence often requires greater precision than demonstrating superiority.
Covariate adjustment addresses this challenge by leveraging baseline characteristics—such as age, disease severity, or genetic markers—that are predictive of the outcome (prognostic covariates). By accounting for these sources of variability in the analysis phase, researchers can isolate the effect of the treatment with greater precision, effectively increasing the signal-to-noise ratio in their experiments [56]. This statistical approach is underutilized despite its potential, partly due to subjective methods for selecting covariates and concerns about model misspecification [57] [56]. Moving toward data-driven, pre-specified adjustment strategies opens a new frontier for increasing statistical power without increasing sample size.
Comparative Analysis of Covariate Adjustment Methods
Several statistical methodologies are available for implementing covariate adjustment in randomized trials. The choice among them depends on the outcome type, the nature of the covariates, and the specific estimand of interest.
Table 1: Key Covariate Adjustment Methods and Their Characteristics
| Method | Core Principle | Best Suited For | Key Considerations |
|---|---|---|---|
| ANCOVA / Direct Regression | Models outcome as a function of treatment and covariates [58] [59]. | Continuous outcomes; Settings with a few, pre-specified covariates. | Highly robust to model misspecification in large samples [58] [60]. |
| G-Computation | Models the outcome, then standardizes predictions over the study population [58]. | Any outcome type; Targeting marginal estimands. | Requires a model for the outcome; more complex implementation. |
| Inverse Probability of Treatment Weighting (IPTW) | Balances covariate distribution via weights based on treatment assignment probability [58]. | Scenarios where outcome modeling is challenging. | Does not require an outcome model; can be inefficient. |
| Augmented IPTW (AIPTW) & Targeted Maximum Likelihood Estimation (TMLE) | Combines outcome and treatment models for double robustness [58]. | Maximizing efficiency and robustness; complex data structures. | Protects against misspecification of one of the two models. |
Performance Comparison: Quantitative Gains in Power and Precision
Empirical evidence from numerous trials consistently demonstrates that covariate adjustment can lead to substantial gains in statistical power, equivalent to a meaningful increase in sample size.
Table 2: Empirical Power and Precision Gains from Covariate Adjustment
| Study / Context | Adjustment Method | Key Outcome | Gain in Power / Precision |
|---|---|---|---|
| CRASH Trial (TBI) [55] | Logistic Regression (IMPACT model) | 14-day mortality | Relative Sample Size (RESS): 0.79 (Power increase from 80% to 88%) |
| CRASH Trial (TBI) [55] | Logistic Regression (CRASH model) | 14-day mortality | Relative Sample Size (RESS): 0.73 (Power increase from 80% to 91%) |
| HCCnet (AI-derived covariate) [56] | Deep Learning-based adjustment | Oncology (HCC) | Power increase from 80% to 85%, or a 12% reduction in required sample size |
| Simulation (Matched Pairs) [61] | Linear Regression with Pair Fixed Effects | Continuous outcomes | Guaranteed weak efficiency improvement over unadjusted analysis |
The Relative Sample Size (RESS) is a key metric for understanding these gains. It is defined as the ratio of the sample size required by an adjusted analysis to that of an unadjusted analysis to achieve the same power. An RESS of 0.79, as seen with the IMPACT model, means a 21% smaller sample size is needed to achieve the same power, a substantial efficiency gain [55].
Experimental Protocols for Covariate Adjustment
Protocol 1: Pre-Specified Regression Adjustment
This is one of the most common and widely recommended approaches for covariate adjustment.
- Covariate Selection: Prior to any analysis, pre-specify a set of baseline covariates that are prognostic for the outcome. This should be based on previous literature, known biology, or external data sources [62] [57]. The strength of the covariate-outcome correlation is the primary criterion for selection.
- Model Specification: For a continuous outcome, use an Analysis of Covariance (ANCOVA) model:
Y_i = α + β * Z_i + γ * X_i + ε_iwhereY_iis the outcome for subjecti,Z_iis the treatment indicator, andX_iis a vector of pre-specified baseline covariates [62]. For binary outcomes, use logistic regression with the same structure. - Estimation: Fit the pre-specified model to the trial data. The treatment effect estimate is the coefficient
β, which represents the effect of treatment while adjusting for the covariates. - Inference: Calculate the standard error and confidence interval for
βto make inferences about the treatment effect. This adjusted analysis will typically yield a narrower confidence interval than an unadjusted analysis.
Protocol 2: Advanced Workflow for Data-Driven Covariate Selection
For trials with a large number of potential covariates, a more advanced, data-driven protocol can be employed to optimize the selection of the most prognostic variables.
This workflow, titled "Data-Driven Covariate Selection," underscores the shift from subjective selection to an optimized, evidence-based process. As noted in the search results, a common pitfall is the subjective selection of covariates based on past practice rather than analytical effort [56]. Leveraging artificial intelligence and machine learning (AI/ML) on external and historical data allows for the identification and ranking of covariates with the highest prognostic strength, such as the HCCnet model which extracts information from histology slides [56]. This ranked list is then used to pre-specify the final covariate set in the trial's statistical analysis plan, guarding against data dredging and ensuring regulatory acceptance.
The Researcher's Toolkit: Essential Reagents for Covariate Adjustment
Successfully implementing covariate adjustment requires both conceptual and practical tools. The following table details key "research reagents" and their functions in this process.
Table 3: Essential Reagents for Implementing Covariate Adjustment
| Category | Item | Function & Purpose |
|---|---|---|
| Statistical Software | R, Python, or Stata | Provides the computational environment to implement ANCOVA, G-computation, IPTW, and other advanced adjustment methods [55] [58]. |
| Prognostic Covariates | Pre-treatment clinical variables (e.g., age, disease severity, biomarkers) | The core "ingredients" for adjustment. These variables explain outcome variation, thereby reducing noise and increasing precision [62] [60]. |
| Pre-Test / Baseline Measure | A measure of the outcome variable taken prior to randomization | Often one of the most powerful prognostic covariates available, as it directly captures the pre-intervention state of the outcome [62]. |
| Statistical Analysis Plan (SAP) | A formal, pre-specified document | The critical "protocol" that details which covariates will be adjusted for and the statistical method to be used, preventing bias from post-hoc data mining [62] [57]. |
| AI/ML Models (Advanced) | Deep learning models (e.g., HCCnet for histology) | Advanced tools to generate novel, highly prognostic covariates from complex data like medical images, pushing the frontier of precision gain [56]. |
Regulatory Landscape and Future Directions
The regulatory environment is increasingly supportive of sophisticated covariate adjustment. The U.S. Food and Drug Administration (FDA) released guidance in May 2023 on adjusting for covariates in randomized clinical trials, providing a formal framework for its application [63]. Furthermore, the European Medicines Agency (EMA) has shown support for innovative approaches, such as issuing a Letter of Support for Owkin's deep learning method to build prognostic covariates from histology slides [56].
The future of this frontier lies in the integration of AI and high-dimensional data. The ability to extract prognostic information from digital pathology, medical imaging, and genomics will create a new class of powerful covariates. This transition from subjective, tradition-based selection to objective, data-driven optimization has the potential to significantly increase the probability of trial success, thereby expediting the delivery of new treatments to patients [56]. For researchers focused on model performance equivalence, mastering these techniques is no longer optional but essential for designing rigorous and efficient studies.
Article Contents
- Introduction to Iterative Refinement: The cyclical engine for model improvement.
- Equivalence Testing in Model Evaluation: The statistical foundation for comparing model performance.
- The Iterative Refinement Cycle in Practice: A step-by-step workflow for researchers.
- Case Study: Equivalence Testing with Model Averaging: Applying the cycle to toxicological gene expression data.
- Quantitative Comparison of Refinement Methodologies: Evaluating different statistical approaches.
- The Researcher's Toolkit: Essential reagents and solutions for equivalence testing.
In the rigorous fields of pharmaceutical development and statistical science, the quest for robust predictive models is not a single event but a continuous process of improvement. This process, known as iterative refinement, is a cyclical methodology for enhancing outcomes through repeated cycles of creation, testing, and revision based on feedback and analysis [64]. At its core, iterative refinement acknowledges that perfection is rarely achieved in a single attempt. Instead, it provides a systematic framework for managing complexity and responding to evolving data and requirements [64]. In the specific context of model equivalence research, iterative refinement transforms model validation from a static checkpoint into a dynamic, evidence-driven learning process.
The principle of iterative refinement aligns closely with modern Agile methodologies, which emphasize iterative flexibility and early, frequent testing over rigid, pre-planned development cycles [65]. This approach is particularly valuable when initial model requirements or the true underlying data-generating processes are not completely clear [64]. By working in iterations, research teams can make progress through a series of small, controlled steps, constantly learning and adjusting along the way to ensure the final model is both robust and well-suited to its purpose [64]. This article will explore how this powerful framework is applied specifically to the problem of establishing statistical equivalence between models, a common challenge in drug development and computational biology.
Equivalence Testing in Model Evaluation
A common problem in numerous research areas, particularly in clinical trials, is to test whether the effect of an explanatory variable on an outcome variable is equivalent across different models or patient groups [26]. Equivalence testing provides a statistical framework for determining whether the performance of two or more models can be considered functionally interchangeable, a key question in model validation and selection. Unlike traditional null hypothesis significance testing that seeks to find differences, equivalence tests are designed to confirm the absence of a practically important difference.
In practice, these tests are frequently used to compare model performance between patient groups, for example, based on gender, age, or treatment regimens [26]. Equivalence is usually assessed by testing whether a chosen performance metric (e.g., prediction accuracy, AUC) or the difference between whole regression curves does not exceed a pre-specified equivalence threshold (Δ) [26]. The choice of this threshold is crucial as it represents the maximal amount of deviation for which equivalence can still be concluded, often based on prior knowledge, regulatory guidelines, or a percentile of the range of the outcome variable [26].
Classical equivalence approaches typically focus on single quantities like means or AUC values [26]. However, when differences depending on a particular covariate are observed, these approaches can lack accuracy. Instead, researchers are increasingly comparing whole regression curves over the entire covariate range (e.g., time windows or dose ranges) using suitable distance measures, such as the maximum absolute distance between curves [26]. This more comprehensive approach is particularly relevant for comparing the performance of complex models across diverse populations or experimental conditions.
The Iterative Refinement Cycle in Practice
Implementing iterative refinement for model equivalence testing follows a structured, recurring cycle. Each cycle builds upon the lessons learned from the previous one, systematically reducing uncertainty and improving model robustness [64]. The process can be visualized as a continuous loop of planning, execution, and learning, designed specifically for the statistical context of model performance evaluation.
The Four-Phase Refinement Cycle
The following workflow diagram illustrates the core iterative refinement cycle for model equivalence testing:
Phase Descriptions and Methodologies
Plan & Design: Before any data collection or analysis, researchers must clearly define the equivalence threshold (Δ) that represents a clinically or practically meaningful difference in model performance [26]. This stage also involves specifying the candidate models to be compared and establishing the primary evaluation metrics. For confirmatory research, pre-registration of these hypotheses and analysis plans is recommended to enhance credibility and reduce researcher degrees of freedom [66].
Execute & Analyze: In this phase, researchers collect experimental data and fit the candidate models. Transparent documentation of all data preprocessing decisions, including outlier handling and missing data management, is critical for reproducibility [66]. Effect sizes and performance metrics should be reported with confidence intervals to convey estimation uncertainty [66].
Test Equivalence: The core analytical phase involves conducting formal equivalence tests comparing model performance against the pre-specified threshold Δ [26]. Both frequentist and Bayesian frameworks can be applied, with the choice depending on the study goals, availability of prior knowledge, and practical constraints [66]. For complex models, approaches based on the distance between entire regression curves may be more appropriate than comparisons of single summary statistics [26].
Refine & Adapt: Based on the equivalence test results, researchers interpret the statistical evidence and make informed decisions about model modifications. This might involve addressing model uncertainty through techniques like model averaging [26], adjusting hyperparameters, or refining the equivalence criteria themselves. The insights gained directly inform the next cycle of planning, completing the iterative loop.
Case Study: Equivalence Testing with Model Averaging
To illustrate the practical application of iterative refinement in model equivalence testing, consider a recent methodological advancement addressing a key challenge: model uncertainty. A 2025 study proposed a flexible equivalence test incorporating model averaging to overcome the critical assumption that the true underlying regression model is known—an assumption rarely met in practice [26].
The Research Challenge
In toxicological gene expression analysis, researchers needed to test the equivalence of time-response curves between two groups for approximately 1000 genes [26]. Traditional equivalence testing approaches required specifying the correct regression model for each gene, which was both time-consuming and prone to model misspecification—a problem that can lead to inflated Type I errors or reduced statistical power [26].
The Iterative Solution
The research team implemented an iterative refinement approach with model averaging at its core:
Initial Cycle: Traditional equivalence tests assuming known model forms showed inconsistent results across genes, with concerns about misspecification bias.
Refinement Insight: Instead of relying on a single "best" model, the team incorporated multiple plausible models using smooth Bayesian Information Criterion (BIC) weights, giving higher weight to better-fitting models while acknowledging model uncertainty [26].
Implementation: The method utilized the duality between confidence intervals and hypothesis testing, deriving a confidence interval for the distance between curves that incorporates model uncertainty [26]. This approach provided both numerical stability and confidence intervals for the equivalence measure.
Experimental Protocol and Workflow
The methodology followed this specific experimental workflow:
Outcomes and Significance
This iterative approach enabled the researchers to analyze equivalence for all 1000 genes without manually specifying each correct model, thus avoiding both a time-consuming model selection step and potential model misspecifications [26]. The model-averaging equivalence test demonstrated robust control of Type I error rates while maintaining good power across various simulation scenarios, showing particular advantage when the true data-generating model was uncertain [26].
Quantitative Comparison of Refinement Methodologies
The effectiveness of different statistical approaches for model equivalence testing can be quantitatively compared across key performance metrics. The following table summarizes experimental data from simulation studies comparing traditional and model-averaging methods:
Table 1: Performance Comparison of Equivalence Testing Methods
| Methodological Approach | Type I Error Control | Statistical Power | Robustness to Model Misspecification | Implementation Complexity |
|---|---|---|---|---|
| Single Model Selection | Variable (often inflated) | High when model correct | Low | Low |
| Model Averaging (BIC Weights) | Good control | Moderately high | High | Medium |
| Frequentist Fixed Sample | Strict control | Moderate | Low | Low |
| Sequential Designs | Strict control | High | Medium | High |
| Bayesian Methods | Good control | High with good priors | Medium with robust priors | Medium |
Data derived from simulation studies in [26] and reporting guidelines in [66].
The table above highlights key trade-offs in methodological selection. Model averaging approaches demonstrate particularly favorable characteristics for iterative refinement contexts, offering a balanced compromise between statistical performance and robustness to uncertainty [26]. The smooth weighting structure based on information criteria (like BIC or AIC) provides stability compared to traditional model selection, where minor data changes can lead to different model choices and consequently different equivalence conclusions [26].
Table 2: Equivalence Testing Decision Framework
| Research Context | Recommended Approach | Key Considerations | Typical Equivalence Threshold (Δ) |
|---|---|---|---|
| Confirmatory Clinical Trials | Pre-registered single model | Regulatory acceptance, simplicity | Based on regulatory guidelines |
| Exploratory Biomarker Studies | Model averaging | High model uncertainty, multiple comparisons | Percentile of outcome variable range |
| Dose-Response Modeling | Curve-based equivalence | Whole profile comparison, not just single points | Maximum acceptable curve distance |
| Model Updating/Validation | Sequential testing | Efficiency, early stopping for equivalence | Clinically meaningless difference |
Framework based on methodologies discussed in [66] [26].
The Researcher's Toolkit
Implementing iterative refinement for model equivalence testing requires both statistical expertise and practical computational tools. The following table details essential "research reagents" and solutions for conducting rigorous equivalence assessments:
Table 3: Essential Research Reagents for Equivalence Testing
| Tool Category | Specific Solution | Primary Function | Implementation Considerations |
|---|---|---|---|
| Statistical Frameworks | R Statistical Environment | Comprehensive data analysis and modeling | Extensive packages for equivalence testing (e.g., TOSTR, equivariance) |
| Equivalence Test Packages | R: simba / R: DoseFinding | Specific implementations for equivalence testing | Support for model averaging and various dose-response models [26] |
| Visualization Tools | ggplot2 / Tableau | Creating transparent result visualizations | Enables clear communication of equivalence test results [67] |
| Simulation Capabilities | Custom R/Python scripts | Assessing operating characteristics | Critical for evaluating Type I error and power [26] |
| Data Management | Electronic Lab Notebooks | Tracking iterative changes | Maintains audit trail of refinement cycles [64] |
Effective iterative refinement for model equivalence testing represents the convergence of rigorous statistical methodology, transparent reporting practices, and computational tooling. By adopting this evidence-based cyclical approach, researchers in drug development and related fields can build more robust, reliable, and generalizable models, ultimately accelerating scientific discovery while maintaining statistical integrity.
In the pursuit of robust statistical inference, researchers face a fundamental methodological choice: should they select a single best model or average across multiple candidate models? This question is particularly critical in fields like pharmaceutical research, where model-based decisions impact drug safety, efficacy, and regulatory approval. This guide provides an objective comparison of Model Selection (MS) and Model Averaging (MA) approaches, examining their theoretical foundations, performance characteristics, and practical applications within model performance equivalence research.
Theoretical Foundations and Comparative Mechanisms
Model Selection and Model Averaging represent two philosophically distinct approaches for handling model uncertainty.
Model Selection aims to identify a single "best" model from a candidate set using criteria like AIC (Akaike Information Criterion) or BIC (Bayesian Information Criterion). The selected model is then treated as if it were the true model for all subsequent inference. [68] AIC is minimax-rate optimal for estimation and does not require the true model to be among the candidates, whereas BIC provides consistent selection when the true model is in the candidate set. [68]
Model Averaging combines estimates from multiple models, explicitly accounting for model uncertainty. Bayesian Model Averaging (BMA) averages models using posterior model probabilities, often approximated via BIC. [68] [26] Frequentist MA methods include Mallows model averaging (MMA), which selects weights to minimize a Mallows criterion, and smooth AIC weighting. [69] [26]
The table below summarizes the core characteristics of each approach:
| Feature | Model Selection (MS) | Model Averaging (MA) |
|---|---|---|
| Core Principle | Selects a single "best" model from candidates [69] | Combines estimates from multiple models [69] |
| Handling Model Uncertainty | Inherently ignores uncertainty in the selection process [69] | Explicitly accounts for and incorporates model uncertainty [69] [26] |
| Primary Theoretical Goals | Asymptotic efficiency; performing as well as the oracle model if known [69] | Combining for adaptation (performing as well as the best candidate) or combining for improvement (beating all candidates) [69] |
| Key Methods | AIC, BIC, Cross-Validation [68] [69] | Bayesian Model Averaging (BMA), Mallows MA (MMA), Smooth AIC/BIC weights [68] [26] |
| Stability | Can be unstable; small data changes may alter selected model [26] | Generally more stable and robust to outliers [26] |
Performance Comparison: Experimental Data and Findings
The relative performance of MS versus MA depends heavily on the underlying data-generating process and model structure.
Key Comparative Findings
Risk Improvement in Nested Models: Under nested linear models, the theoretical risk of an oracle MA is never larger than that of an oracle MS. [70] When the series expansion coefficients of the true regression function decay slowly, the optimal risk of MA can be only a fraction of that of MS, offering significant improvement. When coefficients decay quickly, their risks become asymptotically equivalent. [69]
Approximation Capability: When models are non-nested and a linear combination can significantly reduce modeling biases, MA can outperform MS if the cost of estimating optimal weights is small relative to the bias reduction. This improvement can sometimes be large in terms of convergence rate. [69]
Equivalence Testing Performance: In equivalence testing for regression curves, procedures based on a single pre-specified model can suffer from inflated Type I errors or reduced power if the model is misspecified. Incorporating MA into the testing procedure mitigates this risk, making the test robust to model uncertainty. [26]
The following table summarizes quantitative findings from simulation studies comparing Model Selection and Model Averaging:
| Experiment Scenario | Performance Outcome | Key Interpretation |
|---|---|---|
| Nested Linear Models (Oracle Risk) [70] [69] | MA risk ≤ MS risk; Can be a significant fraction when true coefficients decay slowly | MA can substantially improve estimation risk even without bias reduction advantages |
| Nested Models (Simulation: AIC/BIC vs. MMA) [69] | MMA often outperforms AIC and BIC in terms of estimation risk | The practical benefit of MA is realizable through asymptotically efficient methods |
| Equivalence Testing under Model Uncertainty [26] | MA-based tests control Type I error; model selection-based tests can be inflated | MA provides robustness against model misspecification in hypothesis testing |
| Active Model Selection [71] | CODA method reduces annotation effort by ~70% vs. prior state-of-the-art | Leveraging consensus between models enables highly efficient selection |
Methodological Protocols for Experimental Comparison
To objectively compare MS and MA performance, researchers should implement standardized experimental protocols.
Simulation Study Design for Nested Models
A common protocol examines performance under a known data-generating process: [69]
- Data Generation: Generate data from a linear regression model, often with orthonormal basis functions:
y_i = Σθ_jφ_j(x_i) + ε_i, whereε_iare independent errors with mean 0 and varianceσ². - Candidate Models: Consider a set of nested models, where the
m-th model contains the firstmpredictors. - Estimation: Apply both MS (e.g., AIC, BIC) and MA (e.g., MMA, BMA) methods.
- Performance Evaluation: Compute the empirical risk (e.g., mean squared error) for each method against the true values, often compared to the theoretical risk of oracle MS and MA.
Protocol for Equivalence Testing with Model Uncertainty
To assess equivalence of regression curves (e.g., dose-response) between two groups: [26]
- Specify Model Set: Define a set of candidate models (e.g., linear, Emax, quadratic, exponential, sigmoidal).
- Calculate Model Weights: Fit all candidate models and compute model weights (e.g., based on smooth BIC:
w_m ∠exp(-0.5 * BIC_m)). - Compute Averaged Distance: Calculate a weighted average of the distance (e.g., maximum absolute distance) between the two group curves across all models.
- Perform Test: Compare the model-averaged distance to a pre-specified equivalence threshold using bootstrap to account for parameter uncertainty and obtain critical values.
The following diagram illustrates the core workflow for designing a comparison study between Model Selection and Model Averaging:
Decision Framework and Application Contexts
The choice between MS and MA is not universal but should be guided by the research goals, model structure, and domain context.
When to Prefer Model Selection
- Sparsity Assumption: When you have strong reasons to believe the true model is simple and among the candidates, BIC-based selection is consistent. [68]
- Interpretability is Paramount: When a single, interpretable model is required for decision-making or regulatory explanation. [72]
- Computational Simplicity: When resources are constrained, and averaging over a vast set of models is computationally prohibitive.
When to Prefer Model Averaging
- High Model Uncertainty: When no single model is clearly superior, or multiple models are plausible. [69] [26]
- Prediction Accuracy: The primary goal is minimizing prediction error or estimation risk, as MA reduces variability and can improve performance. [70] [68]
- Robust Inference: When inference needs to be stable and account for model uncertainty, such as in regulatory equivalence tests. [26]
- Non-Nested Models: When candidate models are non-nested, and linear combinations can offer better approximation. [69]
Application in Drug Development (MIDD)
In Model-Informed Drug Development, model uncertainty is prevalent. The "fit-for-purpose" principle aligns the modeling approach with the key question of interest. [72]
- Dose-Response Analysis: MA is increasingly used to robustly identify the dose-response relationship without relying on a single potentially misspecified model. [26]
- Pharmacometric Models: MA helps account for uncertainty in structural model form (e.g., linear, Emax, sigmoid) when predicting clinical outcomes. [72]
The Scientist's Toolkit: Essential Research Reagents
The table below lists key methodological tools and their functions for researchers conducting studies on model selection and averaging.
| Tool Name | Type | Primary Function |
|---|---|---|
| Akaike Information Criterion (AIC) [68] | Model Selection Criterion | Estimates Kullback-Leibler information; minimax-rate optimal for prediction. |
| Bayesian Information Criterion (BIC) [68] [26] | Model Selection Criterion | Approximates posterior model probability; consistent selection under sparsity. |
| Mallows Model Averaging (MMA) [69] | Frequentist MA Method | Selects weights by minimizing a Mallows criterion for asymptotic efficiency. |
| Smooth BIC Weights [26] | Bayesian MA Weights | Approximates Bayesian Model Averaging using BIC to calculate model weights. |
| Focused Information Criterion (FIC) [26] | Model Selection/Averaging Criterion | Selects or averages models based on optimal performance for a specific parameter of interest. |
| Active Model Selection (CODA) [71] | Efficient Evaluation Method | Uses consensus between models and active learning to minimize labeling effort for selection. |
Emerging Trends and Future Directions
The field of model comparison continues to evolve with several promising trends:
- Active Model Selection: New methods like CODA use model consensus and Bayesian inference to drastically reduce the annotation cost of identifying the best model from a candidate pool, showing efficiency gains of 70% or more. [71]
- Integration with AI/ML: Artificial intelligence and machine learning are being leveraged to automate model building, validation, and the selection/averaging process itself, making sophisticated methods more accessible. [72] [73]
- Democratization of Complex Methods: There is a push to develop better user interfaces and software that allow non-specialists, such as clinical leads or regulatory affairs professionals, to apply MA and MS principles effectively within frameworks like Model-Informed Drug Development (MIDD). [73]
Validation, Regulatory Submission, and Comparative Frameworks
The International Council for Harmonisation (ICH) M15 guideline on Model-Informed Drug Development (MIDD) represents a transformative global standard for integrating computational modeling into pharmaceutical development. Endorsed in November 2024, this guideline provides a harmonized framework for planning, evaluating, and reporting MIDD evidence to support regulatory decision-making [74] [75]. MIDD is defined as "the strategic use of computational modeling and simulation (M&S) methods that integrate nonclinical and clinical data, prior information, and knowledge to generate evidence" [76]. This approach enables drug developers to leverage quantitative methods throughout the drug development lifecycle, from discovery through post-marketing phases, facilitating more efficient and informed decision-making [77].
The issuance of ICH M15 marks a pivotal moment in regulatory science, establishing a structured pathway for employing MIDD across diverse therapeutic areas and development scenarios. The guideline aims to align expectations between regulators and sponsors, support consistent regulatory assessments, and minimize discrepancies in the acceptance of modeling and simulation evidence [76]. For researchers and drug development professionals, understanding the principles and applications of ICH M15 is now essential for successful regulatory submissions and optimizing drug development strategies.
The MIDD Framework: Core Principles and Components
Foundational Concepts and Terminology
The ICH M15 guideline establishes a standardized taxonomy for MIDD implementation, centered around several key concepts that form the foundation of a credible modeling approach. The Question of Interest (QOI) defines the specific objective the MIDD evidence aims to address, such as optimizing dose selection or predicting therapeutic outcomes in special populations [78] [77]. The Context of Use (COU) specifies the model's scope, limitations, and how its outcomes will contribute to answering the QOI [78]. This includes explicit statements about the physiological processes represented, assumptions regarding system behavior, and the intended extrapolation domain.
Model Risk Assessment combines the Model Influence (the weight of model outcomes in decision-making) with the Consequence of Wrong Decision (potential impact on patient safety or efficacy) [78] [77]. This risk assessment directly influences the level of evidence needed to establish model credibility, with higher-risk applications requiring more extensive verification and validation. Model Impact reflects the contribution of model outcomes relative to current regulatory expectations or standards, particularly when used to replace traditionally required clinical studies or inform critical labeling decisions [78].
The MIDD Workflow: From Planning to Submission
The MIDD process follows a structured workflow encompassing planning, implementation, evaluation, and submission stages [76] [77]. The initial planning phase involves defining the QOI, COU, and establishing technical criteria for model evaluation, documented in a Model Analysis Plan (MAP). The MAP serves as a pre-defined protocol outlining objectives, data sources, methods, and acceptability standards [77].
Following model development and analysis, comprehensive documentation is assembled in a Model Analysis Report (MAR), which includes detailed descriptions of the model, input data, evaluation results, and interpretation of outcomes relative to the QOI [77]. Assessment tables provide a concise summary linking model outcomes to the QOI, COU, and risk assessments, enhancing transparency and facilitating regulatory review [77]. This structured approach ensures modeling activities are prospectively planned, rigorously evaluated, and transparently reported throughout the drug development lifecycle.
Statistical Equivalence Testing for Model Evaluation
Principles of Equivalence Testing
Within the ICH M15 framework, demonstrating model credibility often requires statistical approaches that prove similarity rather than detect differences. Equivalence testing provides a methodological foundation for establishing that a model's predictions are sufficiently similar to observed data or that two modeling approaches produce comparable results [5]. Unlike traditional statistical tests that aim to detect differences (e.g., t-tests, ANOVA), equivalence testing specifically tests the hypothesis that two measures are equivalent within a pre-specified margin [5].
The core principle of equivalence testing involves defining an Equivalence Acceptance Criterion (EAC), which represents the largest difference between population means that is considered clinically or practically irrelevant [5] [79]. The null hypothesis in equivalence testing states that the differences are large (outside the EAC), while the alternative hypothesis states that the differences are small (within the EAC) [5]. Rejecting the null hypothesis thus provides direct statistical evidence of equivalence.
Implementation Approaches
Two primary methodological approaches implement equivalence testing:
The Two-One-Sided-Tests (TOST) method divides the null hypothesis of non-equivalence into two one-sided null hypotheses (δ ≤ -EAC and δ ≥ EAC) [5]. Each hypothesis is tested with a one-sided test at level α, and the overall null hypothesis is rejected only if both one-sided tests are significant. The p-value for the overall test equals the larger of the two one-sided p-values.
The Confidence Interval Approach establishes equivalence when the 100(1-2α)% confidence interval for the difference in means lies entirely within the equivalence region [5]. For a standard α = 5% equivalence test, this requires the 90% confidence interval to fall completely within the range -EAC to +EAC. This approach provides both statistical and visual interpretation of equivalence results.
Figure 1: Statistical Equivalence Testing Workflow. This diagram illustrates the key decision points in implementing equivalence testing using either the Two-One-Sided-Test (TOST) or Confidence Interval (CI) approach.
Application to Model Credibility Assessment
Equivalence testing provides a rigorous statistical framework for multiple aspects of model evaluation within the ICH M15 framework. For model verification, equivalence testing can demonstrate that model implementations reproduce theoretical results within acceptable numerical tolerances [5]. In model validation, equivalence tests can establish that model predictions match observed clinical data within predefined acceptance bounds [79]. When comparing alternative models, equivalence testing offers a principled approach for determining whether different modeling strategies produce sufficiently similar results to be used interchangeably for specific contexts of use [5].
The application of equivalence testing is particularly valuable for assessing models used in high-influence decision contexts, where the ICH M15 guideline requires more rigorous evidence of model credibility [78] [77]. By providing quantitative evidence of model performance against predefined criteria, equivalence testing directly supports the uncertainty quantification that ICH M15 emphasizes as essential for establishing model credibility [78].
MIDD Methodology Comparison: Approaches and Applications
Spectrum of MIDD Approaches
MIDD encompasses a diverse range of modeling methodologies, each with distinct strengths, applications, and implementation considerations. The ICH M15 guideline acknowledges this diversity and provides a framework for evaluating these approaches based on their specific context of use [76]. The most established MIDD methodologies include Physiologically-Based Pharmacokinetic (PBPK) modeling, Population PK/PD (PopPK/PD), Quantitative Systems Pharmacology (QSP), Exposure-Response Analysis, Model-Based Meta-Analysis (MBMA), and Disease Progression Models [78] [76] [77].
Table 1: Comparison of Major MIDD Methodologies
| Methodology | Primary Applications | Key Strengths | Equivalence Testing Applications |
|---|---|---|---|
| PBPK Modeling | Drug-drug interaction predictions, Special population dosing, Formulation optimization [78] | Incorporates physiological and biochemical parameters; enables extrapolation [78] | Verification against clinical PK data; Comparison of alternative structural models [78] |
| PopPK/PD | Dose selection, Covariate effect identification, Trial design optimization [76] | Accounts for between-subject variability; Sparse data utilization [76] | Model validation against external datasets; Simulation-based validation [5] |
| QSP Modeling | Target validation, Combination therapy, Biomarker strategy [78] | Captures system-level biology; Mechanism-based predictions [78] | Verification of subsystem behavior; Comparison with experimental data [78] |
| Exposure-Response | Dose justification, Benefit-risk assessment, Labeling claims [80] | Direct clinical relevance; Supports regulatory decision-making [80] | Demonstration of similar E-R relationships across populations [5] |
| MBMA | Comparative effectiveness, Trial design, Go/No-go decisions [80] | Integrates published and internal data; Contextualizes treatment effects [80] | Verification against new trial results; Consistency assessment across data sources [5] |
Uncertainty Quantification in Mechanistic Models
For complex mechanistic models such as PBPK and QSP, the ICH M15 guideline emphasizes comprehensive uncertainty quantification (UQ) as essential for establishing model credibility [78]. UQ involves characterizing and estimating uncertainties in both computational and real-world applications to determine how likely certain outcomes are when aspects of the system are not precisely known [78]. The guideline identifies three primary sources of uncertainty in mechanistic models:
Parameter uncertainty emerges from imprecise knowledge of model input parameters, which may be unknown, variable, or cannot be precisely inferred from available data [78]. In PBPK models, this might include tissue partition coefficients or enzyme expression levels. Parametric uncertainty derives from the variability of input variables across the target population, such as demographic factors, genetic polymorphisms, or disease states that influence drug disposition or response [78]. Structural uncertainty (model inadequacy) results from incomplete knowledge of the underlying biology or physics, representing the gap between mathematical representation and the true biological system [78].
The ICH M15 guideline highlights profile likelihood analysis as an efficient tool for practical identifiability analysis of mechanistic models [78]. This approach systematically explores parameter uncertainty and identifiability by fixing one parameter at various values while optimizing all others, revealing how well parameters are constrained by available data. For propagating uncertainty to model outputs, Monte Carlo simulation randomly samples from probability distributions representing parameter uncertainty, running the model with each sampled parameter set and analyzing the resulting distribution of outputs [78].
Experimental Protocols for Model Evaluation
Protocol for Equivalence Testing of Model Predictions
Objective: To demonstrate that model predictions are equivalent to observed clinical data within a predefined acceptance margin.
Materials and Methods:
- Define Equivalence Acceptance Criterion (EAC): Establish the largest difference between model predictions and observed data considered clinically irrelevant, based on scientific knowledge of the therapeutic area and variability of historical data [5] [79].
- Select Statistical Approach: Choose between TOST or confidence interval methods based on study objectives and data characteristics [5].
- Determine Sample Size: Conduct power calculations to ensure adequate sample size for target type I error (typically 5%) and type II error (typically 10-20%) [5] [79].
- Execute Analysis: Perform equivalence testing using the predefined EAC and statistical approach.
- Interpret Results: Conclude equivalence if the test rejects the null hypothesis of non-equivalence (TOST p < 0.05 or 90% CI within EAC bounds) [5].
Acceptance Criteria: Statistical evidence of equivalence (p < 0.05 for TOST or 90% CI completely within EAC bounds) [5].
Protocol for Model Risk Assessment per ICH M15
Objective: To evaluate model risk based on influence and decision consequences as required by ICH M15.
Materials and Methods:
- Define Model Influence: Categorize as low, medium, or high based on the weight of model outcomes in decision-making [78] [77].
- Assess Decision Consequences: Evaluate potential impact on patient safety and efficacy if decisions based on model evidence are wrong [78] [77].
- Determine Model Risk: Combine influence and consequence assessments using the ICH M15 framework [78].
- Define Verification and Validation Activities: Select appropriate evaluation methods commensurate with model risk level [77].
- Document Assessment: Record rationale for risk categorization and corresponding evaluation strategy in the Model Analysis Plan [77].
Acceptance Criteria: Appropriate model evaluation strategy implemented based on risk level, with higher risk models receiving more extensive evaluation [78].
Research Reagent Solutions for MIDD Implementation
Table 2: Essential Research Reagents for MIDD Workflows
| Reagent/Category | Function in MIDD Workflow | Application Examples |
|---|---|---|
| Computational Platforms | Provides environment for model development, simulation, and data analysis [78] [76] | PBPK platform verification; PopPK model development; QSP model simulation [78] |
| Statistical Software | Performs equivalence testing, uncertainty quantification, and statistical analyses [5] | TOST implementation; Profile likelihood analysis; Monte Carlo simulation [78] [5] |
| Clinical Datasets | Serves as reference for model validation and equivalence testing [76] | Model validation against clinical PK data; Exposure-response confirmation [5] [76] |
| Prior Knowledge Databases | Provides foundational information for model structuring and parameterization [78] [76] | Physiological parameter distributions; Disease progression data; Drug-class information [78] |
| Model Documentation Templates | Standardizes MAP and MAR creation per ICH M15 requirements [77] | Study definition; Analysis specification; Result reporting [77] |
Figure 2: MIDD Workflow with Essential Research Reagents. This diagram illustrates the relationship between the key stages of MIDD implementation and the essential research reagents that support each stage.
The implementation of ICH M15 guidelines represents a significant advancement in standardizing the use of modeling and simulation in drug development. By providing a harmonized framework for MIDD planning, evaluation, and documentation, the guideline enables more consistent and transparent assessment of model-derived evidence across regulatory agencies [74] [75] [76]. For researchers and drug development professionals, adherence to ICH M15 principles is increasingly essential for successful regulatory submissions.
Statistical equivalence testing provides a rigorous methodology for demonstrating model credibility within the ICH M15 framework, particularly for establishing that model predictions align with observed data within clinically acceptable margins [5] [79]. When combined with comprehensive uncertainty quantification and appropriate verification and validation activities, equivalence testing strengthens the evidence base supporting model-informed decisions throughout the drug development lifecycle [78].
As MIDD continues to evolve as a critical capability in pharmaceutical development, the ICH M15 guideline establishes a foundation for continued innovation in model-informed approaches. By adopting the principles and practices outlined in this guideline, drug developers can enhance the efficiency of their development programs, strengthen regulatory submissions, and ultimately bring safe and effective medicines to patients more rapidly [80] [76] [77].
In the realm of computational modeling, Verification and Validation (V&V) constitute a fundamental framework for establishing model credibility and reliability. Verification is the process of confirming that a computational model is correctly implemented with respect to its conceptual description and specifications, essentially answering the question: "Did we build the model correctly?" [81]. In contrast, validation assesses how accurately the computational model represents the real-world system it intends to simulate, answering: "Did we build the right model?" [81]. This distinction is critical—verification is primarily a mathematics and software engineering issue, while validation is a physics and application-domain issue [82].
The increasing reliance on "virtual prototyping" and "virtual testing" across engineering and scientific disciplines has elevated the importance of robust V&V processes [82]. As computational models inform key decisions in drug development, aerospace engineering, and other high-consequence fields, establishing model credibility through systematic V&V has become both a scientific necessity and a business imperative [83].
Statistical Equivalence Testing for Model Validation
The Limitation of Traditional Difference Testing
Conventional statistical approaches for evaluating measurement agreement or model accuracy often rely on tests of mean differences (e.g., t-tests, ANOVA). However, this approach is fundamentally flawed for demonstrating equivalence [5]. Failure to reject the null hypothesis of "no difference" does not provide positive evidence of equivalence; it may simply indicate insufficient data or high variability. Conversely, with large sample sizes, even trivial, practically insignificant differences may be detected as statistically significant [5] [7].
Principles of Equivalence Testing
Equivalence testing reverses the conventional statistical hypotheses. The null hypothesis (Hâ‚€) states that the difference between methods is large (non-equivalence), while the alternative hypothesis (Hâ‚) states that the difference is small enough to be considered equivalent [5]. To operationalize "small enough," researchers must define an equivalence region (δ) – the set of differences between population means considered practically equivalent to zero [5]. This region should be justified based on clinical relevance, practical significance, or prior knowledge [5] [7].
The United States Pharmacopeia (USP) chapter <1033> explicitly recommends equivalence testing over significance testing for validation studies, noting that significance tests may detect small, practically insignificant deviations or fail to detect meaningful differences due to insufficient replicates or high variability [7].
Key Methodological Approaches
Two primary statistical methods are used for equivalence testing:
- Two-One-Sided Tests (TOST) Method: This approach tests two one-sided null hypotheses simultaneously: Hâ‚€â‚: δ ≤ -Δ and H₀₂: δ ≥ Δ, where Δ represents the equivalence margin. If both hypotheses are rejected at significance level α, equivalence is concluded [5] [7]. The TOST procedure is visualized in the diagram below:
- Confidence Interval Approach: This method calculates a 100(1-2α)% confidence interval for the difference in means. If the entire confidence interval falls within the equivalence region (-Δ, Δ), equivalence is concluded at the α significance level [5]. For a typical α=0.05 test, a 90% confidence interval is used.
Application in Comparability and Validation Studies
Equivalence testing is particularly valuable for comparability studies in drug development, where process changes must be evaluated for their impact on product quality attributes [7]. The approach follows a systematic workflow:
Table 1: Risk-Based Equivalence Margin Selection in Pharmaceutical Development
| Risk Level | Typical Acceptance Criteria | Application Examples |
|---|---|---|
| High Risk | 5-10% of tolerance or specification | Critical quality attributes with direct impact on safety/efficacy |
| Medium Risk | 11-25% of tolerance or specification | Performance characteristics with indirect clinical relevance |
| Low Risk | 26-50% of tolerance or specification | Non-critical parameters with minimal product impact |
Experimental Protocols for Equivalence Testing
Protocol 1: Equivalence Testing for Method Comparison
This protocol evaluates whether a new measurement method is equivalent to a reference method [5] [7].
Materials and Reagents:
- Reference standard with known value
- Test method instrumentation and reagents
- Appropriate statistical software with equivalence testing capabilities
Procedure:
- Define Equivalence Margin: Establish upper and lower practical limits (UPL and LPL) based on risk assessment and product knowledge (see Table 1).
- Determine Sample Size: Use power analysis to ensure sufficient statistical power (typically 80-90%). For a single mean comparison, the sample size formula is: n = (tâ‚₋α + tâ‚₋β)²(s/δ)² for one-sided tests [7].
- Execute Experimental Runs: Conduct a minimum of n replicate measurements using both reference and test methods.
- Calculate Differences: Subtract reference values from test method measurements.
- Perform Statistical Test: Conduct TOST procedure with practical limits set in step 1.
- Interpret Results: If both one-sided tests are significant (p < 0.05), conclude equivalence.
Protocol 2: Validation of Input-Output Transformations
This protocol validates whether a computational model accurately reproduces real system behavior [81].
Materials:
- Validated computational model
- System input-output data from experimental observations
- Statistical analysis software
Procedure:
- Collect System Data: Record input conditions and corresponding output measures of performance from the actual system.
- Run Model Simulations: Execute the model using the same input conditions recorded in step 1.
- Compare Outputs: Calculate difference between model outputs and system outputs for the performance measure of interest.
- Statistical Analysis: Use hypothesis testing with the test statistic: t₀ = (E(Y) - μ₀)/(S/√n), where E(Y) is the expected model output, μ₀ is the system output, S is standard deviation, and n is sample size [81].
- Alternative Approach: Construct confidence intervals for the difference; if the interval falls entirely within a pre-specified accuracy range, the model is considered valid [81].
Protocol 3: Regression-Based Equivalence Across Multiple Conditions
This protocol evaluates equivalence across a range of experimental conditions or activities using regression analysis [5].
Materials:
- Criterion measurement system
- Test method or model
- Suite of activities or conditions covering expected operating range
Procedure:
- Design Test Matrix: Select a representative suite of conditions (e.g., 23 different physical activities for PA monitor validation [5]).
- Collect Paired Measurements: Obtain criterion and test method measurements across all conditions.
- Fit Regression Model: Establish relationship between test method and criterion (Y = β₀ + βâ‚X + ε).
- Set Equivalence Regions: Define acceptable ranges for intercept (β₀) and slope (βâ‚) parameters.
- Evaluate Equivalence: Check if confidence intervals for β₀ and β₠fall entirely within their respective equivalence regions.
Comparative Analysis of Statistical Approaches
Table 2: Comparison of Statistical Methods for Model Validation
| Method | Null Hypothesis | Interpretation of Non-Significant Result | Appropriate Application | Key Advantages |
|---|---|---|---|---|
| Traditional Significance Test | Means are equal | Cannot reject equality (weak conclusion) | Detecting meaningful differences | Familiar to researchers, widely implemented |
| Equivalence Test (TOST) | Means are different | Reject difference in favor of equivalence (strong conclusion) | Demonstrating practical similarity | Provides direct evidence of equivalence, appropriate for validation |
| Confidence Interval Approach | N/A | Visual assessment of precision | Any scenario requiring equivalence testing | Intuitive interpretation, displays magnitude of effects |
Table 3: Essential Resources for V&V and Equivalence Testing
| Resource Category | Specific Tools/Solutions | Function in V&V Studies |
|---|---|---|
| Statistical Software | R, SAS, Python (SciPy), JMP | Perform TOST procedures, calculate sample size, generate confidence intervals |
| Reference Standards | Certified reference materials, calibrated instruments | Provide known values for method comparison studies |
| Data Collection Tools | Validated measurement systems, electronic data capture | Ensure reliable, accurate raw data for analysis |
| Experimental Design Resources | Sample size calculators, randomization tools | Optimize study design for efficient and conclusive results |
| Documentation Frameworks | Validation master plans, standard operating procedures | Ensure regulatory compliance and study reproducibility |
The integration of equivalence testing principles within the broader V&V framework represents a paradigm shift in how computational models are evaluated and credentialed. Unlike traditional difference testing, which can lead to erroneous conclusions about model validity, equivalence testing provides a statistically rigorous methodology for demonstrating that models are "fit-for-purpose" within defined boundaries [5] [7]. The protocols and comparative analyses presented herein provide researchers and drug development professionals with practical guidance for implementing these methods, ultimately enhancing confidence in computational models that support critical decisions in product design, qualification, and certification [83].
In statistical model validation, a fundamental shift is underway, moving from asking "Are these models different?" to "Are these models similar enough?" [84]. Traditional t-tests have long been the default tool for model comparison, but they address the wrong research question for validation studies [5]. This paradigm shift recognizes that failure to prove difference does not constitute evidence of equivalence [85] [7]. In fields from clinical trial design to ecological modeling, equivalence testing is emerging as the statistically rigorous approach for demonstrating similarity, forcing the burden of proof back onto the model to demonstrate its adequacy rather than merely failing to prove its inadequacy [84].
The limitations of traditional difference testing become particularly problematic in pharmaceutical development and model validation contexts. As noted in BioPharm International, "Failure to reject the null hypothesis of 'no difference' should NOT be taken as evidence that Hâ‚€ is false" [7]. This misconception can lead to erroneous conclusions, especially in studies with small sample sizes or high variability where power to detect differences is limited [5]. Equivalence testing, particularly through the Two One-Sided Tests (TOST) procedure, provides a structured framework for defining and testing what constitutes practically insignificant differences [85] [86].
Conceptual Foundations: Philosophical and Methodological Divides
The Logic of Traditional t-Tests
Traditional independent samples t-tests operate under a null hypothesis (Hâ‚€) that two population means are equal, with an alternative hypothesis (Hâ‚) that they are different [87]. The test statistic evaluates whether the observed difference between sample means is sufficiently large relative to sampling variability to reject Hâ‚€. When the p-value exceeds the significance level (typically 0.05), the conclusion is "failure to reject Hâ‚€" [85]. Critically, this does not prove the means are equal; it merely indicates insufficient evidence to declare them different [7]. This framework inherently favors finding differences when they exist but provides weak evidence for similarity.
The Logic of Equivalence Tests
Equivalence testing fundamentally reverses the conventional hypothesis structure [84] [5]. The null hypothesis becomes that the means differ by at least a clinically or practically important amount (Δ), while the alternative hypothesis asserts they differ by less than this amount:
- H₀: |μ₠- μ₂| ≥ Δ (the difference is practically important)
- Hâ‚: |μ₠- μ₂| < Δ (the difference is practically negligible)
This reversal places the burden of proof on demonstrating equivalence rather than on demonstrating difference [84]. To reject H₀ and claim equivalence, researchers must provide sufficient evidence that the true difference lies within a pre-specified equivalence region [-Δ, Δ] [5].
Defining the Equivalence Region
The most critical aspect of equivalence testing is specifying the equivalence margin (Δ), which represents the largest difference that is considered practically insignificant [5]. This margin should be established based on:
- Clinical or practical relevance: What magnitude of difference would meaningfully impact decisions or outcomes? [7]
- Regulatory guidelines: Established standards for specific applications (e.g., bioequivalence testing)
- Proportion of specification limits: For quality characteristics with specifications, Δ might be set as a percentage of the specification range [7]
- Process capability considerations: The impact on out-of-specification (OOS) rates [7]
For example, in high-risk pharmaceutical applications, equivalence margins might be set at 5-10% of the specification range, while medium-risk applications might use 11-25% [7].
Methodological Comparison: Testing Procedures and Interpretation
The Two One-Sided Tests (TOST) Procedure
The most common equivalence testing approach is the Two One-Sided Tests (TOST) procedure [85] [5]. This method decomposes the composite equivalence null hypothesis into two separate one-sided hypotheses:
- Hâ‚€â‚: μ₠- μ₂ ≤ -Δ
- H₀₂: μ₠- μ₂ ≥ Δ
Both null hypotheses must be rejected at significance level α to conclude equivalence. The corresponding test statistics for the lower and upper bounds are:
\begin{align} t_L = \frac{(\bar{x}_1 - \bar{x}_2) - (-\Delta)}{s_p \sqrt{\frac{1}{n_1} + \frac{1}{n_2}}} \[10pt] t_U = \frac{(\bar{x}_1 - \bar{x}_2) - \Delta}{s_p \sqrt{\frac{1}{n_1} + \frac{1}{n_2}}} \end{align}
where $sp$ is the pooled standard deviation. Both $tL > t{α,ν}$ and $tU < -t_{α,ν}$ must hold to reject the overall null hypothesis of non-equivalence [85] [86].
Figure 1: TOST Procedure Workflow
Confidence Interval Approach
Equivalence testing can also be conducted via confidence intervals [5]. For a significance level α, a 100(1-2α)% confidence interval for the difference in means is constructed:
$$CI{1-2α} = (\bar{x}1 - \bar{x}2) \pm t{α,ν} \cdot sp \sqrt{\frac{1}{n1} + \frac{1}{n_2}}$$
Equivalence is concluded if the entire confidence interval lies within the equivalence region [-Δ, Δ] [5]. For example, with α = 0.05, a 90% confidence interval must fall completely within [-Δ, Δ] to declare equivalence at the 5% significance level.
Comparative Workflows: t-Test vs. Equivalence Testing
Figure 2: Comparison of Testing Approaches
Table 1: Fundamental Differences Between Testing Approaches
| Aspect | Traditional t-Test | Equivalence Test |
|---|---|---|
| Null Hypothesis | Means are equal (H₀: μ₠= μ₂) | Means differ by a meaningful amount (H₀: |μ₠- μ₂| ≥ Δ) |
| Alternative Hypothesis | Means are different (Hâ‚: μ₠≠μ₂) | Means differ by less than Δ (Hâ‚: |μ₠- μ₂| < Δ) |
| Burden of Proof | Evidence must show difference | Evidence must show similarity |
| Interpretation when p > 0.05 | No evidence of difference (inconclusive) | No evidence of equivalence (inconclusive for similarity) |
| Key Parameter | Significance level (α) | Equivalence margin (Δ) and significance level (α) |
| Appropriate Use Case | Detecting meaningful differences | Demonstrating practical similarity |
Applications in Model Validation and Pharmaceutical Sciences
Model Validation Applications
In model validation, equivalence testing provides a rigorous statistical framework for demonstrating that a model's predictions are practically equivalent to observed values or to predictions from a reference model [84]. Robinson and Froese (2004) demonstrated the application of equivalence testing to validate an empirical forest growth model against extensive field measurements, arguing that equivalence tests are more appropriate for model validation because they flip the burden of proof back onto the model [84].
In machine learning comparisons, when evaluating multiple models using resampling techniques, equivalence testing can determine whether performance metrics (e.g., accuracy, RMSE) are practically equivalent across models [88]. This approach acknowledges that in many practical applications, negligible differences in performance metrics should not dictate model selection if other factors like interpretability or computational efficiency favor one model.
Pharmaceutical and Bioequivalence Applications
The pharmaceutical industry has embraced equivalence testing for bioequivalence studies, where researchers must demonstrate that two formulations of a drug have nearly the same effect and are therefore interchangeable [26] [7]. In comparability protocols for manufacturing process changes, equivalence testing assesses whether the change has meaningful impact on product performance characteristics [7].
The United States Pharmacopeia (USP) chapter <1033> explicitly recommends equivalence testing over significance testing for validation studies, stating: "A significance test associated with a P value > 0.05 indicates that there is insufficient evidence to conclude that the parameter is different from the target value. This is not the same as concluding that the parameter conforms to its target value" [7].
Extensions to Regression and Dose-Response Models
Equivalence testing principles extend beyond simple mean comparisons to more complex modeling contexts. In linear regression, equivalence tests can assess whether slope coefficients or mean responses at specific predictor values are practically equivalent [86]. For dose-response studies, researchers have developed equivalence tests for entire regression curves using suitable distance measures [26]. Recent methodological advances incorporate model averaging to address model uncertainty in these equivalence assessments [26].
Table 2: Applications of Equivalence Testing in Scientific Research
| Application Domain | Research Question | Equivalence Margin Considerations |
|---|---|---|
| Model Validation | Are model predictions equivalent to observed values? [84] | Based on practical impact of prediction error |
| Bioequivalence | Do two drug formulations have equivalent effects? [26] | Regulatory standards (often 20% of reference mean) |
| Manufacturing Changes | Does a process change affect product performance? [7] | Risk-based approach (5-50% of specification) |
| Measurement Agreement | Do two measurement methods provide equivalent results? [5] | Clinical decision thresholds or proportion of criterion mean |
| Machine Learning Comparison | Do models have equivalent performance? [88] | Context-dependent meaningful difference in metrics |
Experimental Design and Sample Size Considerations
Power Analysis for Equivalence Tests
Properly designing equivalence studies requires attention to statistical power—the probability of correctly concluding equivalence when the true difference is negligible [52]. Unlike traditional tests where power increases with sample size to detect differences, equivalence test power increases to demonstrate similarity when treatments are truly equivalent.
The sample size for an equivalence test comparing a single mean to a standard value is given by:
$$n = \frac{(t{1-α,ν} + t{1-β,ν})^2(s/δ)^2}{2}$$
where s is the estimated standard deviation, δ is the equivalence margin, α is the significance level, and β is the Type II error rate [7]. This formula highlights that smaller equivalence margins and higher variability require larger sample sizes to achieve adequate power.
Impact of Study Design on Efficiency
Appropriate experimental designs can enhance the efficiency of equivalence assessments. Crossover designs, where each subject receives multiple treatments in sequence, can significantly reduce sample size requirements by controlling for between-subject variability [89]. Grenet et al. found that when within-patient correlation ranges from 0.5 to 0.9, crossover trials require only 5-25% as many participants as parallel-group designs to achieve equivalent statistical power [89].
Covariate adjustment in randomized controlled trials can also improve power for equivalence tests by accounting for prognostic variables [52]. Recent methodological advances have extended prevalent equivalence testing methods to include covariate adjustments, further enhancing statistical power [52].
Implementation Guide: Statistical Tools and Procedures
Research Reagent Solutions: Essential Statistical Tools
Table 3: Essential Components for Implementing Equivalence Tests
| Component | Function | Implementation Considerations |
|---|---|---|
| Equivalence Margin (Δ) | Defines the threshold for practical insignificance | Should be justified based on subject-matter knowledge, not statistical considerations [5] |
| TOST Procedure | Statistical testing framework | Can be implemented using two one-sided t-tests [85] |
| Confidence Intervals | Alternative testing approach | 90% CI for 5% significance test; must lie entirely within [-Δ, Δ] [5] |
| Power Analysis | Sample size determination | Requires specifying Δ, α, power, and estimated variability [7] |
| Software Implementation | Computational tools | R packages (e.g., TOSTER), SAS PROC POWER, Python statsmodels |
Step-by-Step Implementation Protocol
Define the equivalence margin (Δ) based on practical significance: Engage subject-matter experts to establish what difference would be meaningful in the specific application context [7] [5].
Determine sample size using power analysis: Conduct prior to data collection to ensure adequate sensitivity to detect equivalence [7].
Collect data according to experimental design: Consider efficient designs like crossover or blocked arrangements to reduce variability [89] [88].
Perform TOST procedure or construct appropriate confidence interval: Calculate test statistics for both one-sided tests or construct the 100(1-2α)% confidence interval [85] [5].
Draw appropriate conclusions: Reject non-equivalence only if both one-sided tests are significant or the confidence interval falls entirely within [-Δ, Δ] [5].
Report results comprehensively: Include equivalence margin justification, test statistics or confidence intervals, and practical interpretation [7].
Equivalence testing and traditional t-tests address fundamentally different research questions. The choice between them should be guided by the study objectives: difference tests are appropriate when seeking evidence of differential effects, while equivalence tests are proper when the goal is to demonstrate practical similarity [84] [5].
The growing recognition of equivalence testing's importance is reflected in its adoption across diverse fields from pharmaceutical development [7] to ecological modeling [84] and machine learning [88]. Methodological advancements continue to expand its applications, including extensions to regression models [86], dose-response curves [26], and covariate-adjusted analyses [52].
For researchers conducting model validation, equivalence testing provides the statistically rigorous framework needed to properly demonstrate that model predictions are practically equivalent to observed values or to outputs from reference models [84]. By defining equivalence margins based on practical significance rather than statistical conventions, and by placing the burden of proof on demonstrating similarity rather than on demonstrating difference, equivalence testing offers a more appropriate paradigm for validation studies than traditional difference testing.
In the stringent world of pharmaceutical and medical device development, a Model Analysis Plan (MAP) serves as a critical blueprint for the statistical evaluation of complex models intended for regulatory submission. This document provides an objective framework for comparing the performance of a candidate model against established alternatives, ensuring that the chosen model is not only predictive but also rigorously validated and defensible in the eyes of regulatory authorities. The MAP is a specialized extension of the broader Statistical Analysis Plan (SAP), which is a foundational document outlining the planned statistical methods and procedures for analyzing data from a clinical trial [90]. For researchers, scientists, and drug development professionals, a well-constructed MAP moves beyond simply demonstrating that a model works; it provides conclusive, statistically sound evidence that the model's performance is equivalent or superior to existing standards, thereby supporting its use in critical decision-making for product approval.
The strategic importance of this document cannot be overstated. A high-quality MAP, completed alongside the study protocol, can identify design flaws early, optimize sample size, and introduce rigor into the study design [91]. Ultimately, it functions as a contract between the project team and regulatory agencies, ensuring transparency and adherence to pre-specified analyses, which is a cornerstone of regulatory compliance and reproducible research [90] [91].
Statistical Foundations: Testing for Equivalence in Model Performance
When comparing models, the conventional statistical approach of using tests designed to find differences (e.g., t-tests, ANOVA) is fundamentally flawed. A non-significant p-value from such a test does not prove equivalence; it may simply indicate an underpowered study [5]. Equivalence testing, conversely, is specifically designed to provide evidence that two methods are sufficiently similar.
The Principles of Equivalence Testing
In equivalence testing, the traditional null and alternative hypotheses are reversed. The null hypothesis (H0) becomes that the two models are not equivalent (i.e., the difference in their performance is large). The alternative hypothesis (H1) is that they are equivalent (i.e., the difference is small) [5]. To operationalize "small," investigators must pre-define an equivalence region (also called a region of indifference), which is the range of differences between model performance metrics considered clinically or practically insignificant [30] [5].
Key Methods: TOST and Confidence Intervals
The most common method for testing equivalence is the Two-One-Sided-Tests (TOST) procedure [5]. This method tests two simultaneous one-sided hypotheses to determine if the true difference in performance is greater than the lower equivalence limit and less than the upper equivalence limit.
An equivalent and highly intuitive approach is the confidence interval method. Here, the null hypothesis of non-equivalence is rejected at the 5% significance level if the 90% confidence interval for the difference in performance metrics lies entirely within the pre-specified equivalence region [5]. This relationship between confidence intervals and equivalence testing provides a clear visual and statistical means for assessing model comparability.
Building Your Model Analysis Plan: A Practical Framework
A robust MAP should be finalized early in the model development process, ideally during the trial design phase and before data collection begins, to prevent bias and ensure clear objectives [90]. The following table outlines the core components of a comprehensive MAP.
| MAP Component | Description | Considerations for Model Comparison |
|---|---|---|
| Introduction & Study Overview | Background information and model objectives. | State the purpose of the model comparison and the role of each model (e.g., candidate vs. reference). |
| Objectives & Hypotheses | Primary, secondary, and exploratory objectives; precise statistical hypotheses. | Pre-specify the performance metrics and formally state the equivalence hypotheses and region. |
| Model Specifications | Detailed description of all models being compared. | Define the model structures (e.g., linear, EMax, machine learning algorithms), parameters, and software. |
| Performance Endpoints | The metrics used to evaluate and compare model performance. | Common metrics include RMSE, AIC, BIC, C-index, or AUC. Justify the choice of metrics. |
| Equivalence Region | The pre-specified, justified range of differences considered "equivalent." | This is a critical decision based on clinical relevance, prior knowledge, or regulatory guidance. |
| Statistical Methods | Detailed analytical procedures for the comparison. | Specify the use of TOST, confidence intervals, and methods for handling missing data or multiplicity. |
| Data Presentation | Plans for TLFs (Tables, Listings, and Figures). | Include mock-ups of summary tables and plots (e.g., Bland-Altman, confidence intervals). |
| Sensitivity Analyses | Plans to assess the robustness of the conclusions. | Describe analyses using different equivalence margins or handling of outliers. |
Incorporating the Estimands Framework
For clinical trials, the estimands framework (ICH E9 R1) brings additional clarity and precision to a MAP. An estimand is a precise description of the treatment effect, comprising the population, variable, and how to handle intercurrent events [90]. When comparing models, the estimand framework ensures that the model's purpose and the handling of complex scenarios (e.g., treatment discontinuation) are aligned with the trial's scientific question, thereby guaranteeing that the performance comparison is meaningful for regulatory interpretation [90].
Experimental Protocols for Model Comparison
Protocol 1: Equivalence Testing for a Continuous Performance Metric
This protocol is suitable when comparing models based on a continuous error metric, such as Root-Mean-Square Error (RMSE) or mean bias.
- Define the Equivalence Region (δ): Prior to analysis, define the equivalence margin. For example, equivalence for a new predictive model might be declared if its RMSE is within 0.5 units of the reference model's RMSE.
- Calculate the Performance Difference: For each model, calculate the performance metric (e.g., RMSE) on a validation dataset. The observed difference (θ) is: RMSE_candidate - RMSE_reference.
- Construct a Confidence Interval: Calculate the 90% confidence interval (CI) for the true difference in performance.
- Perform the Equivalence Test: Apply the TOST procedure. If the 90% CI for θ lies entirely within the interval [-δ, +δ], the null hypothesis of non-equivalence is rejected, and the models are considered statistically equivalent.
Protocol 2: Cross-Validation for Survival Model Performance
This protocol is adapted from research comparing classical statistical models with machine learning models for survival data [92]. It is ideal for low-dimensional data and models like the Fine-Gray model versus Random Survival Forests.
- Data Partitioning: Split the dataset into 5 folds of equal size.
- Cross-Validation Loop: Repeat the following 5 times:
- Hold out one fold as the validation set.
- Train both models on the remaining 4 folds.
- Generate predictions on the validation set and calculate the performance metric (e.g., C-index or Brier score).
- Repeat the holdout procedure a second time using the same 5 folds but with a different fold used for validation, resulting in 2 estimates per repetition (5x2-fold cv) [92].
- Statistical Testing: Use a specialized test, such as the 5x2-fold cv paired t-test or the combined 5x2-fold cv F-test, on the collected performance metrics to determine if the observed difference in performance is statistically significant [92].
The workflow for a rigorous model comparison, from data preparation to regulatory interpretation, is summarized in the following diagram.
Essential Research Reagent Solutions for Model Analysis
The following table details key statistical and computational tools required for executing a rigorous model comparison as part of a MAP.
| Research Reagent / Tool | Function in Model Analysis |
|---|---|
| Statistical Software (R, Python, SAS) | Provides the computational environment for fitting models, calculating performance metrics, and executing statistical tests like equivalence testing. |
| Equivalence Testing Library (e.g., TOST in R) | A dedicated statistical library for performing Two-One-Sided-Tests (TOST) and calculating corresponding confidence intervals and p-values. |
| Cross-Validation Framework | A tool for partitioning data and automating the training/validation cycle to obtain robust, unbiased estimates of model performance. |
| Model Averaging Algorithms | Advanced techniques to account for model uncertainty by combining estimates from multiple candidate models, rather than relying on a single selected model [26]. |
| Geostatistical Analysis Module (e.g., ArcGIS) | For spatial models, this provides specialized comparison statistics (e.g., standardized RMSE) to determine the optimal predictive surface [93]. |
| Electronic Data Capture (EDC) System | Ensures the integrity and traceability of the source data used to develop and validate the models, a key regulatory requirement. |
A meticulously crafted Model Analysis Plan is more than a technical requirement; it is a strategic asset in the regulatory submission process. By adopting a framework centered on equivalence testing, researchers can move beyond simply showing a model works to providing definitive evidence that it performs as well as, or better than, accepted standards. This approach, combined with early planning, clear documentation, and adherence to regulatory guidelines like ICH E9, ensures that model development is transparent, rigorous, and ultimately successful in gaining regulatory approval.
Demonstrating Equivalence for Compendial Methods and Alternative Procedures
In the pharmaceutical industry, demonstrating that an alternative analytical procedure is equivalent to a compendial method is a critical requirement for regulatory compliance and operational efficiency. This process ensures that drug substances and products consistently meet established acceptance criteria for their intended use, forming the foundation of a robust quality control strategy [94] [95]. The International Council for Harmonisation (ICH) defines a specification as "a list of tests, references to analytical procedures, and appropriate acceptance criteria" which constitute the critical quality standards approved by regulatory authorities as conditions of market authorization [94] [95].
The fundamental principle for demonstrating equivalence, as outlined by the Pharmacopoeial Discussion Group (PDG) and adapted for this purpose, is that "a pharmaceutical substance or product tested by the harmonized procedure yields the same results and the same accept/reject decision is reached" regardless of the analytical method employed [94]. This guide provides a comprehensive framework for designing, executing, and interpreting equivalence studies, incorporating advanced statistical methodologies and practical implementation strategies relevant to researchers, scientists, and drug development professionals.
Regulatory Framework and Key Concepts
Regulatory Foundations
The demonstration of method equivalence operates within a well-defined regulatory landscape. Key guidelines include:
- ICH Q2(R2) and ICH Q14: Provide the validation requirements and scientific approaches for analytical procedure development and maintenance [95]
- USP General Chapters: <1010> offers statistical tools for equivalency protocols, while <1223> specifically addresses validation of alternative microbiological methods [95] [96]
- European Pharmacopoeia Chapter 5.27: "Comparability of Alternative Analytical Procedures" outlines the process for demonstrating comparability to pharmacopoeial methods [97]
- FDA Guidance for Industry: "Analytical Procedures and Method Validation for Drugs and Biologics" provides requirements for method comparability studies [98]
Regulatory authorities universally require that any alternative method must be fully validated and produce comparable results to the compendial method within established allowable limits [98]. The European Pharmacopoeia specifically mandates that "the use of an alternative procedure is subject to authorization by the competent authority" [97], emphasizing the importance of rigorous demonstration of comparability.
Defining Specification Equivalence
Specification equivalence encompasses both the analytical procedures and their associated acceptance criteria [94]. This comprehensive approach involves:
- Method Equivalence: Demonstration that alternative and compendial procedures produce statistically equivalent results
- Acceptance Criteria Equivalence: Confirmation that the same accept/reject decisions are reached for the material being tested [94]
The concept of "harmonization by attribute" enables manufacturers to perform risk assessments attribute by attribute to ensure equivalent decisions regardless of the analytical method used [94]. This approach is particularly valuable when entire monographs cannot be fully harmonized across different pharmacopoeias.
Table 1: Core Components of Specification Equivalence
| Component | Definition | Regulatory Basis |
|---|---|---|
| Method Equivalence | Demonstration that two analytical procedures produce statistically equivalent results | USP <1010>, Ph. Eur. 5.27 [95] [97] |
| Acceptance Criteria Equivalence | Confirmation that the same accept/reject decisions are reached | PDG Harmonization Principle [94] |
| Decision Equivalence | The frequency of positive/negative results is non-inferior to the compendial method | USP <1223> [96] |
| Performance Equivalence | Alternative method demonstrates equivalent or better validation parameters | FDA Guidance on Alternative Methods [98] |
Statistical Approaches for Equivalence Testing
Foundational Statistical Concepts
Equivalence testing employs specialized statistical methodologies that differ fundamentally from conventional hypothesis testing. Where traditional tests seek to detect differences, equivalence tests aim to confirm the absence of clinically or analytically meaningful differences [26]. The key statistical concepts include:
- Equivalence Threshold (Δ): A pre-specified boundary representing the maximum acceptable difference between methods that still allows conclusion of equivalence [26]
- Confidence Interval Approach: Equivalence is demonstrated when the confidence interval for the difference between methods falls entirely within the equivalence interval [-Δ, +Δ]
- Type I Error (α): The probability of incorrectly declaring equivalence when methods are not equivalent, typically set at 0.05
- Power (1-β): The probability of correctly declaring equivalence when methods are truly equivalent, typically targeted at 80% or higher
Advanced approaches address scenarios where traditional equivalence testing assumptions may not hold, particularly when differences depend on specific covariates. In such cases, testing single quantities (e.g., means) may be insufficient, and instead, whole regression curves over the entire covariate range are considered using suitable distance measures [26].
Addressing Model Uncertainty through Model Averaging
A significant challenge in equivalence testing arises when the true underlying regression model is unknown, which can lead to inflated Type I errors or reduced power [26]. Model averaging provides a flexible solution that incorporates model uncertainty directly into the testing procedure.
The model averaging approach uses smooth weights based on information criteria [26]:
- Smooth AIC Weights: Frequentist model averaging using Akaike Information Criterion
- Smooth BIC Weights: Bayesian model averaging using Bayesian Information Criterion
- Focused Information Criterion (FIC): Model averaging focused directly on the parameter of primary interest
This approach is particularly valuable in dose-response and time-response studies where multiple plausible models may exist, and selecting a single model may introduce bias or instability in the equivalence conclusion [26].
Diagram 1: Statistical Workflow for Equivalence Testing with Model Uncertainty
Experimental Design and Protocols
Prerequisites for Equivalence Studies
Before initiating equivalence testing, specific prerequisites must be satisfied to ensure valid results:
- Method Validation: Both methods must be fully validated according to current regulatory standards (ICH Q2(R2)) with demonstrated accuracy, precision, specificity, and robustness [94] [95]
- Method Verification: The receiving laboratory must demonstrate proper implementation through method verification or transfer protocols [94]
- System Suitability: Both methods must meet system suitability criteria prior to and during the equivalence study
The European Pharmacopoeia Chapter 5.27 emphasizes that "demonstration that the alternative procedure meets its performance criteria during validation is not sufficient to imply comparability with the pharmacopoeial procedure" [97]. The performance of both procedures must be directly assessed and compared through a structured study.
Study Design Considerations
A well-designed equivalence study incorporates these key elements:
- Sample Selection: Representative samples covering the entire specification range, including samples near critical quality attributes
- Sample Size: Sufficient replicates to provide adequate statistical power (typically 3 independent preparations with multiple determinations each)
- Randomization: Random order of analysis to minimize systematic bias
- Blinding: Where possible, analysts should be blinded to the method being used to prevent conscious or unconscious bias
Table 2: Experimental Design Parameters for Equivalence Studies
| Parameter | Minimum Recommendation | Optimal Design | Statistical Consideration |
|---|---|---|---|
| Sample Lots | 3 | 5-6 | Represents manufacturing variability |
| Independent Preps | 3 | 3-6 | Accounts for preparation variability |
| Replicates per Prep | 2-3 | 3-6 | Estimates method precision |
| Concentration Levels | 3 (low, medium, high) | 5 across range | Evaluates response across range |
| Total Determinations | 15-20 | 30-50 | Provides adequate power for equivalence testing |
Method Suitability Testing
For microbiological methods, method suitability must be established for each product matrix to demonstrate "absence of product effect that would cover up or influence the outcome of the method" [96]. This involves:
- Product Interference Testing: Demonstrating that product components don't inhibit or enhance microbial recovery
- Challenge Organisms: Using appropriate representative microorganisms based on product bioburden
- Recovery Comparison: Quantitative methods require accuracy and precision validation, while qualitative methods focus on challenge organism recovery [96]
Equivalence Demonstration Approaches
Four Frameworks for Equivalence
Alternative methods can be demonstrated as equivalent through four distinct approaches, each with specific application domains and evidence requirements [96]:
- Acceptable Procedure: Uses reference materials with known properties to prove acceptability
- Performance Equivalence: Requires equivalent or better results for validation criteria (accuracy, precision, specificity, detection limits)
- Results Equivalence: Direct comparison of numerical results between methods with established tolerance intervals
- Decision Equivalence: Demonstration of equivalent pass/fail decisions rather than numerical equivalence
Diagram 2: Four Approaches for Demonstrating Method Equivalence
Statistical Analysis Methods
The statistical approach depends on the type of data and the equivalence framework being applied:
For Continuous Data (Results Equivalence):
- Equivalence Testing: Two one-sided tests (TOST) procedure
- Bland-Altman Analysis: Assessment of bias and agreement limits
- Linear Regression: Evaluation of slope, intercept, and confidence intervals
- Tolerance Intervals: Comparison of results against pre-defined acceptance limits
For Categorical Data (Decision Equivalence):
- Cohen's Kappa (κ): Measures agreement beyond chance [99]
- McNemar's Test: Assesses marginal homogeneity in paired binary data
- Proportion Agreement: Simple percentage agreement with pre-defined acceptable limits
Advanced approaches may incorporate model averaging to address uncertainty in the underlying data structure, using smooth weights based on information criteria (AIC, BIC) to improve the robustness of equivalence conclusions [26].
Implementation and Documentation
Change Control and Regulatory Submissions
Implementing an alternative method requires careful change control management:
- Regulatory Assessment: Determination of impact on approved marketing authorization filings
- Change Control Documentation: Formal documentation of the change through the quality system
- Submission Strategy: Regulatory submission to relevant health authorities when required
- Approval Timing: Implementation only after receiving necessary regulatory approvals [95]
The significance of method changes determines the regulatory pathway. "A change that impacts the method in the approved marketing dossier must be submitted to the health authorities for some level of approval prior to implementation" [95].
Documentation Requirements
Comprehensive documentation is essential for demonstrating equivalence:
- Protocol Development: Pre-approved study protocol detailing acceptance criteria and statistical approaches
- Raw Data Retention: Complete records of all testing performed
- Statistical Analysis Report: Detailed explanation of statistical methods and justification of choices
- Validation Report: Summary of method validation status for both procedures
- Equivalence Conclusion: Formal statement of equivalence with supporting evidence
The European Pharmacopoeia emphasizes that "the final responsibility for the demonstration of comparability lies with the user and the successful outcome of the process needs to be demonstrated and documented to the satisfaction of the competent authority" [97].
Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Equivalence Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Reference Standards | Method calibration and system suitability | Certified reference materials with documented traceability |
| Challenge Microorganisms | Method suitability testing (microbiological methods) | Representative strains including ATCC cultures |
| Matrix-Blanked Samples | Specificity and interference assessment | Placebo formulations without active ingredient |
| Quality Control Samples | Precision and accuracy assessment | Samples with known concentrations spanning specification range |
| Extraction Solvents | Sample preparation and recovery studies | Appropriate for product matrix and method requirements |
Demonstrating equivalence between compendial and alternative methods requires a systematic approach integrating rigorous experimental design, appropriate statistical methodologies, and comprehensive documentation. The framework presented enables pharmaceutical scientists to develop robust equivalence protocols that meet regulatory expectations while facilitating method improvements and technological advancements.
The application of advanced statistical approaches, including model averaging to address model uncertainty, enhances the robustness of equivalence conclusions, particularly for complex analytical procedures where multiple plausible models may exist [26]. By adhering to the principles outlined in this guide and leveraging the appropriate equivalence demonstration strategy for their specific context, researchers can successfully implement alternative methods that maintain product quality while potentially offering advantages in accuracy, sensitivity, precision, or efficiency [98] [96].
Conclusion
Equivalence testing provides a robust statistical framework for demonstrating that model performances are practically indistinguishable, a crucial need in drug development where model-based decisions impact regulatory approvals and patient safety. By integrating foundational principles like TOST with advanced methods such as model averaging, researchers can effectively navigate model uncertainty. Adhering to emerging regulatory standards like ICH M15 ensures that model validation is both scientifically sound and compliant. Future directions will likely see greater integration of these methods with AI/ML models and more sophisticated power analysis techniques, further solidifying the role of equivalence testing as a cornerstone of rigorous, model-informed biomedical research.
References
- 1. Statistical Significance vs. Equivalence: What Clinical ... [https://www.medxteam.de/en/medxteam-blog/how-to-create-a-clinical-assessment-based-on-performance-data-2]
- 2. Understanding P-Values and Statistical Significance [https://www.simplypsychology.org/p-value.html]
- 3. 9 Equivalence Testing and Interval Hypotheses - GitHub Pages [https://lakens.github.io/statistical_inferences/09-equivalencetest.html]
- 4. Statistical significance: p value, 0.05 threshold, and ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-020-0145-y]
- 5. A Primer on the Use of Equivalence Testing for Evaluating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5856600/]
- 6. Statistical Equivalence and Test-Retest Reliability of Delay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4116793/]
- 7. Equivalence Testing for Comparability [https://www.biopharminternational.com/view/equivalence-testing-comparability]
- 8. Statistical and regulatory considerations in assessments of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4046084/]
- 9. A Practical Primer for t Tests, Correlations, and Meta-Analyses [https://pmc.ncbi.nlm.nih.gov/articles/PMC5502906/]
- 10. Equivalence and non-inferiority trials in the evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406809/]
- 11. Bioequivalence Criteria & Requirements [https://www.biopharmaservices.com/services-support/bioequivalence-criteria-and-requirements-explained/]
- 12. Bioavailability and Bioequivalence in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC4157693/]
- 13. Equivalence Testing for F-tests • TOSTER [https://aaroncaldwell.us/TOSTERpkg/articles/the_ftestTOSTER.html]
- 14. Estimands in equivalence trials and non-inferiority trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-025-09068-2]
- 15. B-Value and Empirical Equivalence Bound [https://pmc.ncbi.nlm.nih.gov/articles/PMC8881334/]
- 16. Two One-Sided Test (TOST) Procedure [https://www.emergentmind.com/topics/two-one-sided-test-tost-procedure]
- 17. Equivalence Testing (TOST) [https://real-statistics.com/students-t-distribution/equivalence-testing-tost/]
- 18. Equivalence trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9106130/]
- 19. Introduction to Equivalence Testing with TOSTER [https://cran.rstudio.com/web/packages/TOSTER/vignettes/IntroductionToTOSTER.html]
- 20. An Introduction to t_TOST • TOSTER [https://aaroncaldwell.us/TOSTERpkg/articles/IntroTOSTt.html]
- 21. 21 CFR Part 320 -- Bioavailability and Bioequivalence ... [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-D/part-320]
- 22. Statistical Approaches to Establishing Bioequivalence [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/statistical-approaches-establishing-bioequivalence]
- 23. 15.12 - Bioequivalence Trials | STAT 509 [https://online.stat.psu.edu/stat509/lesson/15/15.12]
- 24. 16.2 Two One-Sided Tests Equivalence Testing [https://bookdown.org/mike/data_analysis/sec-two-one-sided-tests-equivalence-testing.html]
- 25. Model Uncertainty - an overview [https://www.sciencedirect.com/topics/engineering/model-uncertainty]
- 26. How Equivalence Tests Can Benefit From Model Averaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC11923417/]
- 27. Understanding Model Uncertainty in Machine Learning [https://imerit.net/resources/blog/a-comprehensive-introduction-to-uncertainty-in-machine-learning-all-una/]
- 28. Uncertainty quantification [https://en.wikipedia.org/wiki/Uncertainty_quantification]
- 29. A Review and Classification of Model Uncertainty [https://arxiv.org/html/2508.07864v1]
- 30. Model validation using equivalence tests [https://www.sciencedirect.com/science/article/abs/pii/S0304380004000985]
- 31. Optimal designs for frequentist model averaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6690170/]
- 32. Model Averaging for Left-Truncated Reinsurance Losses [https://variancejournal.org/article/141749]
- 33. Optimal Designs for Model Averaging in non-nested Models [https://link.springer.com/article/10.1007/s13171-020-00238-9]
- 34. Model Averaging with AIC Weights for Hypothesis Testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5495511/]
- 35. Bayesian Model Weighting: The Many Faces of ... [https://www.mdpi.com/2073-4441/12/2/309]
- 36. Model averaging based on generalized method of moments [https://www.sciencedirect.com/science/article/abs/pii/S0165176521000124]
- 37. how equivalence tests can benefit from model averaging [https://arxiv.org/html/2405.00827v1]
- 38. An empirical approach to sufficient similarity - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/23398277/]
- 39. Bootstrapping (statistics) [https://en.wikipedia.org/wiki/Bootstrapping_(statistics)]
- 40. Comparing Alternative Corrections for Bias in the Bias ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8988747/]
- 41. Re-evaluation of the comparative effectiveness of bootstrap ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7789544/]
- 42. Model Misspecification [https://www.cfainstitute.org/insights/professional-learning/refresher-readings/2025/model-misspecification]
- 43. A cautionary tale of model misspecification and identifiability [https://arxiv.org/html/2507.04894v3]
- 44. Statistical Tests for Comparing Possibly Misspecified and ... [https://pubmed.ncbi.nlm.nih.gov/10733862/]
- 45. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 46. Real-World Data and Causal Machine Learning to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579681/]
- 47. Power for equivalence tests - Minitab - Support [https://support.minitab.com/en-us/minitab/help-and-how-to/statistics/power-and-sample-size/supporting-topics/power-for-equivalence-tests/]
- 48. Chapter 11 Equivalence tests and sample size | Welcome! [https://dstanley4.github.io/psyc4780bookdown/equivalence-tests-and-sample-size.html]
- 49. Power and sample size procedures for equivalence ... [https://link.springer.com/article/10.1007/s42519-025-00494-8]
- 50. Establishing Process Equivalency: A Practical Guide [https://www.propharmagroup.com/thought-leadership/establishing-process-equivalency]
- 51. Equivalence test and confidence interval for the difference ... [https://pubmed.ncbi.nlm.nih.gov/9595618/]
- 52. Statistical Power for Equivalence Tests in Randomized ... [https://eval25.eventscribe.net/ajaxcalls/PresentationInfo.asp?efp=Tk5KVEtBTkoyNTAyMw&PresentationID=1680681&rnd=0.5511364]
- 53. Confidence intervals in equivalence testing - Support - Minitab [https://support.minitab.com/en-us/minitab/help-and-how-to/statistics/equivalence-tests/supporting-topics/confidence-intervals-in-equivalence-testing/]
- 54. Testing for equivalence with confidence intervals or P values [https://www.graphpad.com/guides/prism/latest/statistics/stat_testing_for_equivalence_with_c.htm]
- 55. Covariate adjustment increased power in randomized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3589911/]
- 56. clinical trial benefits with advanced covariate adjustment [https://www.nature.com/articles/d42473-023-00245-y]
- 57. Simple Rules for Improving Clinical Trial Confidence with ... [https://pubmed.ncbi.nlm.nih.gov/40618828/]
- 58. A comparison of covariate adjustment approaches under ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9817411/]
- 59. Covariate Adjustment in Randomized Clinical Trials with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094063/]
- 60. Covariate adjustment in trials [https://www.mrcctu.ucl.ac.uk/our-research/methodology/analysis/covariate-adjustment-in-trials/]
- 61. Covariate adjustment in experiments with matched pairs [https://www.sciencedirect.com/science/article/abs/pii/S0304407624000861]
- 62. 10 Things to Know About Covariate Adjustment [https://methods.egap.org/guides/analysis-procedures/covariates_en.html]
- 63. Adjusting for Covariates in Randomized Clinical Trials ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/adjusting-covariates-randomized-clinical-trials-drugs-and-biological-products]
- 64. Iterative Refinement → Term [https://fashion.sustainability-directory.com/term/iterative-refinement/]
- 65. An iterative, interdisciplinary, collaborative framework for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7796712/]
- 66. Improving statistical reporting in psychology [https://www.nature.com/articles/s44271-025-00356-w]
- 67. Guide to Item Comparison: Elevate Your Data Presentation ... [https://www.storytellingwithcharts.com/blog/the-ultimate-guide-to-item-comparison-elevate-your-data-presentation-skills/]
- 68. Model Selection and Model Averaging [https://www.stat.umn.edu/geyer/5421/notes/glmbb.html]
- 69. On improvability of model selection by model averaging [https://www.sciencedirect.com/science/article/abs/pii/S0304407620303973]
- 70. A COMPARISON FOR NESTED LINEAR MODELS [https://www.cambridge.org/core/journals/econometric-theory/article/from-model-selection-to-model-averaging-a-comparison-for-nested-linear-models/E8B5CDEB9AD2E437A3C3C8278EFAA288]
- 71. Consensus-Driven Active Model Selection [https://arxiv.org/html/2507.23771v1]
- 72. Advancing drug development with “Fit-for-Purpose†modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 73. CERTAINTY 2025: The power of Model-Informed Drug ... [https://www.certara.com/blog/certainty-the-power-of-model-informed-drug-development/]
- 74. M15 General Principles for Model-Informed Drug ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m15-general-principles-model-informed-drug-development]
- 75. M15 General Principles for Model-Informed Drug ... [https://www.federalregister.gov/documents/2024/12/30/2024-31027/m15-general-principles-for-model-informed-drug-development-international-council-for-harmonisation]
- 76. Scoping review of the role of pharmacometrics in model- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528282/]
- 77. MIDD: Decoding the ICH M15 Guideline [https://www.linkedin.com/pulse/midd-decoding-ich-m15-guideline-chandramouli-r-fnrlc]
- 78. Mechanistic Modeling in Model-Informed Drug Development [https://investigationsquality.com/2025/03/10/mechanistic-modeling-in-model-informed-drug-development-regulatory-compliance-under-ich-m15/]
- 79. Demonstrating Comparability of Stability Profiles Using ... [https://www.biopharminternational.com/view/demonstrating-comparability-stability-profiles-using-statistical-equivalence-testing]
- 80. Regulatory Strategy: Insights from the Draft ICH M15 ... [https://www.certara.com/blog/redefining-regulatory-strategy-with-midd-insights-from-the-draft-ich-m15-guidance/]
- 81. Verification and validation of computer simulation models [https://en.wikipedia.org/wiki/Verification_and_validation_of_computer_simulation_models]
- 82. Verification and validation in computational fluid dynamics [https://www.sciencedirect.com/science/article/abs/pii/S0376042102000052]
- 83. Verification, Validation, Uncertainty Quantification in ... [https://www.nafems.org/events/nafems/2025/verification-and-validation-in-engineering-simulation-online-01/?srsltid=AfmBOorGEBJZvDCwzY6w1q4wwaBt4z6UZE6Inupw0i280Rj0palCQ526]
- 84. Model validation using equivalence tests [https://digitalcommons.mtu.edu/michigantech-p/6306/]
- 85. Equivalence Testing vs t-Test: Why Failing to Reject Hâ‚€ ... [https://medium.com/@stathacks/equivalence-testing-vs-t-test-why-failing-to-reject-h%E2%82%80-doesnt-mean-h%E2%82%80-is-true-a7d0d91f8296]
- 86. On the Equivalence Test and Sample Size Procedures for ... [https://link.springer.com/article/10.1007/s44199-024-00089-5]
- 87. A simple guide to the use of Student's t-test, Mann-Whitney U ... [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-025-00465-6]
- 88. 14 Comparing Models [https://aml4td.org/chapters/comparing-models.html]
- 89. Equivalence Test and Sample Size Determination Based ... [https://www.mdpi.com/2075-1680/14/8/582]
- 90. How to Understand and Create a Statistical Analysis Plan ... [https://www.quanticate.com/blog/how-to-understand-and-create-a-statistical-analysis-plan]
- 91. A template for the authoring of statistical analysis plans - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10300078/]
- 92. Statistical approaches to identifying significant differences in ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0279435]
- 93. Comparing models - ArcMap Resources for ArcGIS Desktop [https://desktop.arcgis.com/en/arcmap/latest/extensions/geostatistical-analyst/comparing-models.htm]
- 94. Specification Equivalence—A Practical Approach [https://www.pharmtech.com/view/specification-equivalence-a-practical-approach]
- 95. Specification Equivalence: A Practical Approach to Method ... [https://www.biopharminternational.com/view/specification-equivalence-a-practical-approach-to-method-and-acceptance-criteria-equivalence]
- 96. What Are Method Suitability Testing & Method Equivalency ... [https://www.linkedin.com/pulse/what-method-suitability-testing-equivalency-mycoscience]
- 97. New Ph. Eur. Chapter Comparability of Alternative ... [https://www.gmp-compliance.org/gmp-news/new-ph-eur-chapter-comparability-of-alternative-analytical-procedures]
- 98. Are All Methods Equivalent? [https://www.lachmanconsultants.com/2019/10/are-all-methods-equivalent/]
- 99. Evaluation metrics and statistical tests for machine learning [https://www.nature.com/articles/s41598-024-56706-x]