Harmonizing Genomic Medicine: Strategies to Resolve Interlaboratory Differences in Variant Interpretation
Inconsistent classification of genetic variants across clinical laboratories presents a significant challenge in genomic medicine, with reported discordance rates of 10-40%.
Harmonizing Genomic Medicine: Strategies to Resolve Interlaboratory Differences in Variant Interpretation
Abstract
Inconsistent classification of genetic variants across clinical laboratories presents a significant challenge in genomic medicine, with reported discordance rates of 10-40%. This article provides researchers, scientists, and drug development professionals with a comprehensive framework to understand, address, and minimize these inconsistencies. We explore the foundational causes of interpretation differences, detail established and emerging methodological standards from ACMG/AMP and ClinGen, and offer practical troubleshooting strategies for optimization. The content further covers validation techniques and comparative analyses of computational tools, culminating in a forward-looking synthesis that underscores the critical role of data sharing, gene-specific guidelines, and advanced bioinformatics in achieving reproducible and clinically actionable variant classification.
Understanding the Inconsistency Problem: Scope and Root Causes in Genomic Interpretation
Interlaboratory discordance—the variation in results when the same sample is analyzed by different laboratories—presents a significant challenge in biomedical research and clinical diagnostics. This inconsistency can affect a wide range of fields, from genetic testing and cancer diagnosis to serology and neurobiology, potentially impacting research reproducibility, patient diagnosis, and treatment decisions. This guide quantifies the scope of this problem, presents key experimental data, and provides actionable troubleshooting protocols for researchers and scientists to identify, manage, and reduce discordance in their own work.
### FAQs: Understanding Interlaboratory Discordance
1. How common is diagnostic discordance in pathology? Studies reveal that initial diagnostic discordance can be surprisingly high. One investigation into breast pathology found that when comparing expert review with original database diagnoses, the initial overall discordance rate was 32.2% (131 of 407 cases). However, by applying a systematic 5-step framework to identify and correct for data errors and borderline cases, this discordance was reduced to less than 10% [1]. Another study focusing on breast cancer biomarkers (ER, PR, HER2, Ki-67) found pathological discordance rates ranging from 28% to 38.1% when comparing biopsies from the same patient under different conditions (e.g., pre- and post-chemotherapy, or between different institutions) [2].
2. What are the rates of discordance in genetic variant interpretation? Discordance is a recognized issue in clinical genetics. An initiative by the Canadian Open Genetics Repository (COGR) found that among variants classified by two or more laboratories, 34.4% had discordant interpretations when using a standard five-tier classification model (Pathogenic, Likely Pathogenic, VUS, Likely Benign, Benign). This discordance was significantly reduced to 29.9% after laboratories participated in a structured data-sharing and reassessment process. When viewed through the lens of clinical actionability (a two-tier model), the discordance was much lower, falling from 3.2% to 1.5% after reassessment [3]. A separate pilot of the ACMG-AMP guidelines showed that initial concordance across laboratories can be as low as 34%, though this can be improved to 71% through consensus discussions and detailed review of the criteria [4].
3. Which types of samples or tests are most prone to discordance?
Discordance is more likely in non-typical or borderline cases. In HER2 FISH testing for breast cancer, while overall agreement among laboratories can be substantial, cases with characteristics near the critical cutoff range or with genetic heterogeneity show significantly lower congruence, poorer reproducibility, and higher variability [5]. Similarly, in Alzheimer's disease biomarker research, a small but consistent percentage (around 6%) of patients show discordant results between cerebrospinal fluid (CSF) analysis and amyloid PET imaging, often associated with factors like APOE ε4 carriage and mixed or non-AD pathologies [6].
4. What are the primary causes of interlaboratory discordance? The causes are multifaceted and can include:
- Data Errors: Simple errors in data abstraction or entry can account for a portion of initial discordance. One study found that 2.9% of cases had data errors originating from the underlying registry, incomplete slides, or data abstraction [1].
- Interpretive Subjectivity: Differences in how pathologists or scientists interpret the same data or images is a key factor. One study concluded that the evaluating center and pathologist are important reasons for observed differences in breast biopsy immunohistochemistry [2].
- Pre-analytical and Analytical Variability: Differences in sample handling, reagents, assay conditions, and testing platforms contribute to variability. This is a noted issue in CSF biomarker analysis for Alzheimer's disease [6].
- Borderline Cases: Cases that naturally fall on the borderline between two diagnostic categories are a major source of disagreement. Among cases with clinically meaningful discordance, 53% were considered borderline [1].
- Evolution of Evidence and Guidelines: In genetics, classifications can change over time as new evidence emerges or guidelines are updated, leading to discordance if laboratories assess the same variant at different times [3].
### Quantitative Data on Discordance Rates
The tables below summarize key quantitative findings on interlaboratory discordance from recent studies.
Table 1: Diagnostic Discordance Rates in Pathology and Serology
| Field / Condition | Type of Test / Sample | Initial Discordance Rate | Discordance Rate After Review/QA | Key Contributing Factors |
|---|---|---|---|---|
| Breast Pathology [1] | Diagnostic categorization (benign, DCIS, invasive cancer) | 32.2% | < 10% | Data errors, borderline cases, interpretive variation |
| Breast Cancer Biomarkers [2] | IHC (ER, PR, HER2, Ki-67) between biopsies | 28.0% - 38.1% | Not Reported | Neoadjuvant therapy, tumor heterogeneity, evaluating center/pathologist |
| HER2 FISH Testing [5] | Gene amplification (all samples) | -- | Fleiss' κ: 0.765-0.911* | -- |
| HER2 FISH Testing [5] | Gene amplification (borderline/heterogeneous samples) | -- | Fleiss' κ: 0.582* | Lack of validation, lack of standard procedures, signals near cutoff |
| Serology [7] | ELISA re-testing | Variable (see example) | -- | Kit performance, laboratory quality |
*Fleiss' kappa is a statistical measure of inter-rater reliability where >0.8 is almost perfect agreement, 0.6-0.8 is substantial, and 0.4-0.6 is moderate.
Table 2: Discordance Rates in Genetic Variant Interpretation [3]
| Classification Model | Description | Baseline Discordance | Discordance After Reassessment |
|---|---|---|---|
| Five-Tier Model | Pathogenic, Likely Pathogenic, VUS, Likely Benign, Benign | 34.4% | 29.9% |
| Three-Tier Model | Positive (P/LP), Inconclusive (VUS), Negative (LB/B) | 16.7% | 11.5% |
| Two-Tier Model | Actionable (P/LP), Not Actionable (VUS/LB/B) | 3.2% | 1.5% |
### Troubleshooting Guides & Experimental Protocols
Guide 1: A Framework for Evaluating Diagnostic Discordance in Research
This 5-step framework, adapted from a study on breast pathology, provides a systematic method to identify and address discordance uncovered during research activities [1].
Step-by-Step Protocol:
Compare the Expert Review and Database Diagnoses: [1]
- Objective: To quantify the initial level of discordance.
- Action: Have an independent expert, blinded to the original diagnosis, review the source material (e.g., pathology slides, genetic data). Compare this expert diagnosis to the diagnosis recorded in your research database.
- Documentation: Carefully oversee research staff conducting these comparisons and document all findings.
Determine the Clinical Significance of Diagnostic Discordance: [1]
- Objective: To prioritize cases that require further investigation.
- Action: Categorize the discordance based on its potential impact. For example, would the different diagnoses lead to different treatment recommendations? Focus subsequent review on cases with "clinically meaningful" discordance.
- Documentation: Consult clinical experts as needed and document the rationale for significance categorizations.
Identify and Correct Data Errors and Verify True Diagnostic Discordance: [1]
- Objective: To distinguish true interpretive differences from simple data errors.
- Action: For discordant cases, go back to the original source data (e.g., original pathology reports, raw sequencing data). Check for abstraction errors, coding errors, or issues with sample quality/completeness.
- Documentation: Correct any data errors and document all changes. The remaining discordances are likely "true" interpretive differences.
Consider the Impact of Borderline Cases: [1]
- Objective: To understand how cases that naturally fall between categories affect discordance rates.
- Action: Review study documents to identify cases that were explicitly noted as borderline by either the original interpreter or the expert. Analyze the extent to which these cases contribute to the overall discordance.
- Documentation: Apply agreed-upon definitions for borderline cases and document their frequency.
Determine the Notification Approach for Verified Discordant Diagnoses: [1]
- Objective: To ethically manage the discovery of significant discordances that may impact past research or clinical care.
- Action: Consider the time lag since the original analysis and consult with experts in research ethics and relevant clinical fields to decide on a course of action, which may include notifying the original laboratory or facility.
- Documentation: Document all notification methods and practices.
Guide 2: Protocol for Handling Discordant and Equivocal Results in Serological Testing
This protocol provides a clear hierarchy for managing discordant or equivocal results from repeated testing, such as in seroprevalence studies. [7]
Experimental Workflow:
Re-test a Stratified Subset: Select a subset of specimens for re-testing that includes all equivocal results, a random subset of negative results, and a random subset of positive results from the first run. The second test can use the same kit or a different one, and may be performed in a different laboratory.
Construct a Concordance Table: Build a 3x3 table (Positive, Negative, Equivocal) comparing the results from the first and second runs to assess overall concordance.
Determine Overall Run Validity: If the concordance analysis shows a significant number of results that change categories (e.g., positive to negative), this casts doubt on the quality of the first run, and all specimens from that run should be re-analyzed.
Assign Final Outcome Values: For individual specimens with discordant results, follow a pre-specified hierarchy. An example hierarchy is:
- Use the results from the first run if its quality has been validated.
- Initial equivocal results may be replaced with positive or negative results obtained from a subsequent, validated run.
- For specimens that remain equivocal after re-testing, the study protocol must pre-specify how to categorize them (e.g., count as positive, count as negative, or maintain a separate category).
### The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Materials for Discordance Resolution in Genetic and Pathology Research
| Reagent / Solution | Function in Discordance Resolution | Example Use Case |
|---|---|---|
| Digital Pathology Platforms [8] | Enables remote expert review, proficiency testing, and creation of permanent digital archives for re-evaluation, reducing slide handling damage and logistical issues. | National quality assurance programs in cytopathology using whole-slide imaging for diagnostic proficiency testing. |
| Variant Interpretation Platforms (e.g., Franklin by Genoox) [3] | AI-based tools that aggregate evidence from multiple sources and provide a suggested variant classification, facilitating comparison and consensus-building across laboratories. | Canadian Open Genetics Repository (COGR) using Franklin to identify and resolve discordant variant interpretations between labs. |
| Automated CSF Assay Platforms (e.g., Lumipulse) [6] | Reduce inter-laboratory variability by automating biomarker analysis, leading to higher consistency compared to manual ELISA assays. | Cross-platform comparison of Alzheimer's disease biomarkers (Aβ42, p-tau) to improve concordance with amyloid PET. |
| Standardized Antibody Panels [2] | Using validated, consistent antibody clones and staining protocols across laboratories minimizes a major source of technical variability in IHC. | Ensuring consistent staining for ER, PR, HER2, and Ki-67 in breast cancer biomarker studies. |
| Cell Line-Derived Quality Control Materials [5] | Provide homogeneous, well-characterized control materials with known results for proficiency testing and assay validation. | Using breast carcinoma cell lines (BT474, HCC1954) to create FFPE QC materials for HER2 FISH ring studies. |
FAQs: Understanding Interlaboratory Differences in Variant Interpretation
What are the main types of interpretation discrepancies?
Interlaboratory differences in variant classification are categorized by their potential impact on clinical management [9]:
- Five-tier class inconsistency: A difference among the five specific classification categories: Pathogenic (P), Likely Pathogenic (LP), Variant of Uncertain Significance (VUS), Likely Benign (LB), and Benign (B).
- Three-tier class inconsistency: A difference among the three broader classification levels: P/LP vs. VUS vs. LB/B.
- Medically Significant Difference (MSD): A difference between actionable and non-actionable variants, specifically P/LP versus VUS/LB/B. This is the most critical type of discrepancy as it can directly influence patient care [9].
How prevalent are these inconsistencies?
Reported rates of interpretation differences vary, but studies highlight a significant challenge. The table below summarizes key findings from published literature [9].
| Study | Number of Variants | Disease Context | Initial Inconsistent Rate | Rate After Resolution Efforts |
|---|---|---|---|---|
| Amendola et al., 2016 [9] | 99 | Unlimited | 66% (Five-tier) | 29% (Five-tier) |
| Garber et al., 2016 [9] | 293 | Neuromuscular, Skeletal | 56.7% (Five-tier) | Not Mentioned |
| Harrison et al., 2017 [10] | 6,169 | Unlimited | 11.7% (Three-tier) | 8.3% (Three-tier) |
| Amendola et al., 2020 [9] | 158 | 59 Genes | 16% (Five-tier) | Not Mentioned |
One multi-laboratory study found that 87.2% of discordant variants were resolved after reassessment with current criteria and internal data sharing, while 12.8% remained discordant primarily due to differences in applying the ACMG-AMP guidelines [10].
What core factors drive these discrepancies?
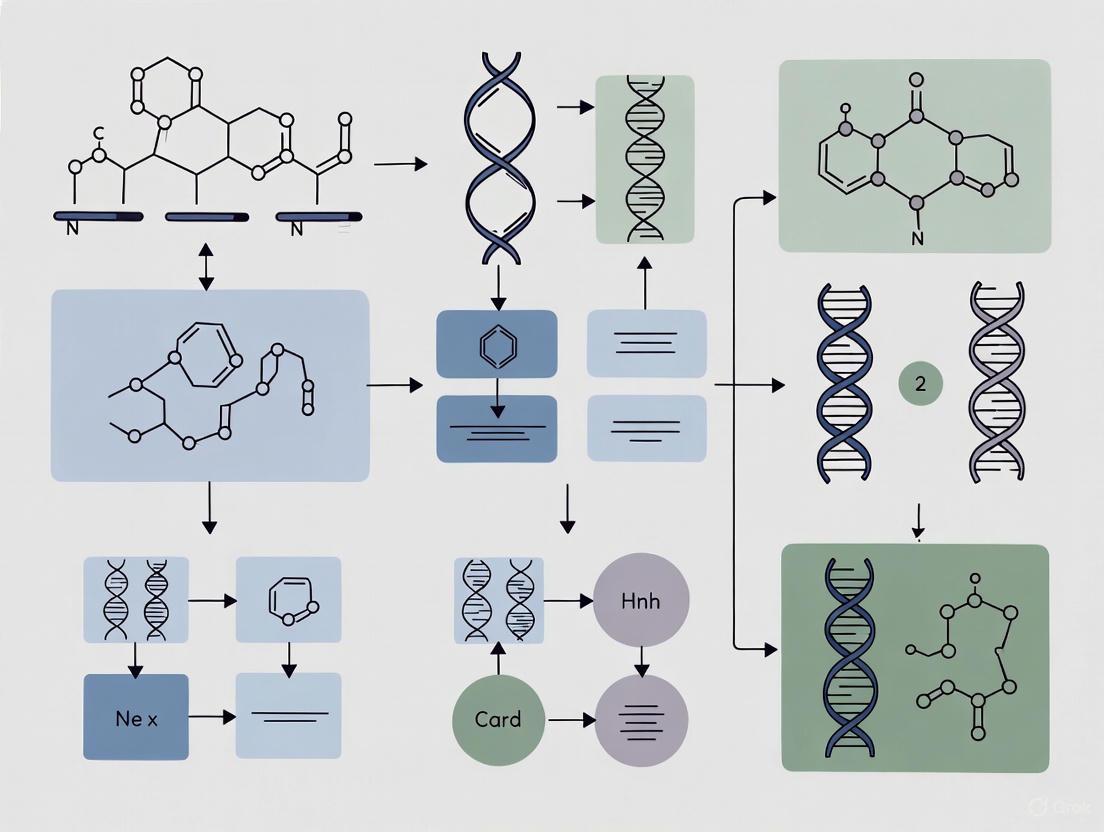
Discrepancies arise from multiple points in the interpretation workflow, illustrated in the following diagram.
Classification Methodology
Historically, many clinical laboratories developed their own in-house interpretation protocols, leading to inherent differences in classification pathways [9]. While the 2015 ACMG/AMP guideline standardized the framework, its design for broad adaptability means some criteria lack absolute precision. For example, laboratories may set different thresholds for allele frequency when applying the "extremely low frequency" (PM2) criterion, such as 0.1%, 0.5%, or 1% [9].
Asymmetric Information
Differences in the information available to interpreters is a primary cause of discrepancies [9]. This includes:
- Analysis Timeframe: Laboratories analyzing the same variant at different times may have access to different versions of public databases and literature.
- Internal Data: Access to private, internal laboratory data, such as allele frequencies from internal cohorts or previously classified cases, is often not uniformly shared [10].
- Phenotypic Information: Accurate use of phenotype-specificity (PP4) criteria relies on comprehensive and accurate clinical information, which can be limited or atypical at the time of testing [9].
Discordant Evidence Application
Even with the same evidence, laboratories may apply the ACMG/AMP criteria differently. A key study found that for variants that remained discordant after reassessment and data sharing, the root cause was "differences in the application of the ACMG-AMP guidelines" [10]. This reflects subjectivity in weighing and combining different types of evidence.
Subjective Expert Judgement
The ACMG/AMP guidelines require interpreters to combine multidimensional evidence with personal experience [9]. This necessary expert judgment introduces an inherent level of subjectivity, particularly when evidence is conflicting or novel scenarios are encountered.
Experimental Protocol: Systematic Variant Reassessment to Resolve Discrepancies
The following workflow, based on a successful multi-laboratory collaboration, provides a detailed methodology for identifying and resolving interpretation differences [10].
Key Procedures:
- Identification & Prioritization: Systematically compare variant classifications from multiple laboratories using a shared database like ClinVar. Prioritize reassessment based on clinical impact, focusing first on Medically Significant Differences (P/LP vs. LB/B), then on P/LP vs. VUS differences [10].
- Data Sharing and Documentation: For each prioritized variant, laboratories should confidentially share internal data (e.g., allele counts, co-segregation data, functional assay results) and fully document the initial rationale for classification, including the specific ACMG/AMP criteria used [10].
- Independent Reassessment: Each laboratory performs a new classification based on all pooled evidence and the current version of the ACMG/AMP guidelines. This step should be done independently before comparing results [10].
- Root Cause Analysis: For variants that remain discordant after reassessment, the specific points of disagreement in the application of the ACMG/AMP criteria must be identified and documented. This highlights areas where the guidelines may require further refinement or clarification [10].
The following tools and databases are essential for consistent and accurate variant interpretation.
| Resource Name | Type | Primary Function in Variant Interpretation |
|---|---|---|
| ACMG/AMP Guidelines [9] [10] | Interpretation Framework | Provides the standardized evidence-based framework for classifying variants into P, LP, VUS, LB, and B categories. |
| ClinVar [10] | Public Database | A central, public archive for submissions of interpreted variants, allowing for identification of interpretation differences between labs. |
| Population Databases (e.g., gnomAD) | Data Resource | Provides allele frequency data in healthy populations, critical for applying frequency-based criteria (e.g., PM2, BS1). |
| Internal Laboratory Database | Proprietary Data | Contains a laboratory's cumulative internal data on allele frequency and observed phenotypes, a common source of informational asymmetry [10]. |
| * Phenotypic Curation Tools* | Methodology | Standardized methods for capturing and relating patient clinical features to genetic findings, crucial for accurate PP4/BP4 application [9]. |
The Impact of Evolving Guidelines and Asymmetric Information
In genetic research, a critical challenge is the consistent classification of DNA variants across different laboratories. Interlaboratory variation in variant interpretation poses a significant barrier to reliable diagnostics and drug development. Differences in the application of evolving professional guidelines and asymmetric information—where one lab possesses data another does not—are primary drivers of these discrepancies. This technical support center provides targeted guidance to help researchers identify, troubleshoot, and resolve these issues, thereby enhancing the reproducibility and reliability of their findings.
The Scale of the Problem: Quantitative Evidence
Understanding the frequency and nature of interpretation differences is the first step in addressing them. The following table summarizes key findings from analyses of public variant databases.
| Metric | Findings | Source/Context |
|---|---|---|
| Overall Discordance Rate | 47.4% (2,985 of 6,292 variants) had conflicting interpretations [10]. | Variants interpreted by ≥2 clinical laboratories [10]. |
| Clinically Substantial Discordance | 3.2% (201 of 6,292 variants) had interpretations crossing the pathogenic/likely pathogenic vs. benign/likely benign/VUS threshold [11] [10]. | Conflicts with potential to directly impact clinical management [11]. |
| Discordance in Therapeutically Relevant Genes | 58.2% (117 of 201) of clinically substantial conflicts occurred in genes with therapeutic implications [11]. | Conflicts affect treatment decisions for conditions like epilepsy [11]. |
| Resolution through Data Sharing | 87.2% (211 of 242) of initially discordant variants were resolved after reassessment with current criteria and/or internal data sharing [10]. | Collaborative reanalysis demonstrated high resolvability [10]. |
Troubleshooting Guides & FAQs
Guide 1: Diagnosing the Source of Interpretation Differences
Use this workflow to systematically identify the root cause of a variant classification discrepancy between your lab and an external source.
Frequently Asked Questions
Q1: Our lab has classified a variant as a "Variant of Uncertain Significance (VUS)," but another reputable lab calls it "Likely Pathogenic." What immediate steps should we take?
A1: Follow this protocol:
- Contact the Other Laboratory: Initiate a direct dialogue to share the specific evidence and reasoning behind your respective classifications. This is the most effective first step [10].
- Conduct an Internal Reassessment: Re-evaluate the variant using the most current version of the ACMG/AMP guidelines and all available internal data.
- Share Internal Data Formally: If the discrepancy persists after initial discussion, propose a structured data sharing agreement. Collaborative studies have shown that sharing internal data (e.g., case observations, functional data) resolves a majority of interpretation differences [10].
- Submit to ClinVar: Report your final interpretation, along with supporting evidence, to the public ClinVar database. Note any discrepancies with other submitters to contribute to global resolution efforts [11] [10].
Q2: How can we proactively minimize interpretation differences when establishing a new testing protocol?
A2: Implement these practices from the outset:
- Adopt Latest Standards: Mandate the use of the most recent professional guidelines (e.g., current ACMG/AMP standards) and ensure all analysts are trained on their consistent application.
- Define a Data-Sharing Charter: For multi-center research, establish a pre-approved agreement for sharing internal variant data to reduce information asymmetry.
- Use Public Databases: Require that all variant interpretations and supporting evidence are submitted to ClinVar, fostering transparency and crowd-sourced peer review [10].
- Implement Periodic Review: Schedule regular re-analysis of variant classifications to incorporate new public evidence and evolving guidelines.
Q3: What is the role of regulatory guidelines and data standards in mitigating this problem?
A3: Evolving regulatory and data standards are crucial for creating a more transparent and consistent ecosystem.
- Clinical Trial Protocols: The updated SPIRIT 2025 statement emphasizes protocol completeness, including plans for data sharing and transparent description of methods, which underpins reproducible research [12].
- Data Standards: Regulatory bodies like the FDA require standardized data formats (e.g., CDISC standards) for submissions. Using these standards from the research phase improves data quality, traceability, and facilitates sharing and comparison across studies [13] [14].
- Real-World Evidence (RWE): Regulatory agencies are increasingly accepting RWE. Developing standards for incorporating RWE into variant interpretation can help resolve conflicts by providing additional, large-scale data points [15] [16].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents, databases, and platforms are essential for conducting robust variant interpretation research and implementing the troubleshooting guides above.
| Tool / Resource | Function / Application |
|---|---|
| ClinVar Database | Public archive of reports on the relationships between human variations and phenotypes, with supporting evidence. Used to compare your interpretations with other labs [11] [10]. |
| ACMG/AMP Guidelines | An evidence-based framework for classifying sequence variants into categories like "Pathogenic," "Likely Pathogenic," "VUS," "Likely Benign," and "Benign." Provides a standardized starting point for interpretation [10]. |
| CDISC Standards | Foundational and therapeutic area-specific data standards. Their use ensures data is structured consistently, which is critical for sharing, pooling, and comparing data across laboratories and for regulatory submissions [13] [14]. |
| Bioinformatics Pipelines | Software for processing next-generation sequencing data, performing variant calling, and annotation. Standardized pipelines help reduce technical sources of variation before clinical interpretation. |
| Internal Laboratory Database | A curated, private database of a lab's own historical variant interpretations and associated patient and functional data. A key source of information that can create asymmetry if not shared [10]. |
Experimental Protocol: Resolving a Specific Variant Interpretation Discrepancy
This detailed methodology is adapted from published collaborative efforts and provides a step-by-step guide for reconciling a specific variant interpretation difference between two or more laboratories [10].
Objective: To achieve consensus on the clinical classification of a specific genetic variant where interpretations between laboratories differ.
Materials:
- Variant of interest (e.g., GRCh38 genomic coordinates).
- Access to public data resources (ClinVar, gnomAD, PubMed, locus-specific databases).
- Access to internal laboratory data (case observations, functional data, family studies).
- Current ACMG/AMP classification guidelines and any relevant disease-specific modifications.
Procedure:
- Variant Identification and Initial Assessment:
- Identify the variant for which a interpretation discrepancy exists.
- Each laboratory involved should document their current classification and, critically, compile the complete evidence matrix used to reach that conclusion. This includes listing every ACMG/AMP criterion that was applied and its strength (e.g., PM1, PP3, BS1).
Blinded Evidence Comparison:
- In a structured meeting or exchange, the laboratories should share the types of evidence they considered (e.g., "we used population data from gnomAD," "we have two unrelated affected cases," "we applied the PP3 in-silico prediction criterion") without initially revealing the final calculated classification.
- This helps identify differences in the evidence base (information asymmetry) versus differences in how the same evidence was weighted.
Structured Data Sharing and Reassessment:
- Share any unique internal data (e.g., detailed clinical phenotypes of probands, segregation data, functional assay results) that was previously held by only one laboratory.
- Each laboratory then independently re-assesses the variant using the now-shared complete evidence set and the current ACMG/AMP guidelines.
Consensus Discussion:
- Compare the new, post-reassessment classifications.
- If discrepancies remain, focus the discussion on the specific ACMG/AMP criteria where application differs. For example, one lab may have applied a "Strong" (PS4) criterion for multiple observed cases, while another applied a "Moderate" (PM1) criterion for the same data.
- The goal is to understand the subjective differences in guideline application.
Finalization and Reporting:
- Document the final consensus classification, or agree to disagree and document the respective positions with clear rationales.
- Update internal laboratory databases.
- Submit the new interpretation(s) and the shared evidence that led to it to ClinVar. This closes the loop and informs the global community, preventing future redundant investigations [10].
Technical Support Center
Troubleshooting Guides
Guide 1: Resolving Discordant Variant Classifications
Problem: Different laboratories classify the same sequence variant differently, leading to conflicting clinical reports.
Solution:
- Assemble a Multidisciplinary Committee: Form a variant interpretation committee (VIC) comprising clinical geneticists, molecular biologists, bioinformaticians, and pathologists [17].
- Adopt a Standardized Scheme: Implement a five-tier classification system (e.g., the IARC system endorsed by the Human Variome Project) [17].
- Define Rigorous Criteria: Establish transparent, evidence-based criteria for each classification tier. Require multiple lines of evidence, including clinical, genetic, and functional data, to support any classification [17].
- Aggregate Data via Microattribution: Use a centralized locus-specific database (LSDB) and encourage data submission through microattribution to credit contributors, which helps resolve classifications for variants with scarce data [17].
- Reach Consensus: Hold regular committee meetings to review evidence and assign a final consensus classification for each variant [17].
Guide 2: Addressing Failure to Meet Analytical Performance Requirements
Problem: Laboratory results for specific analytes do not meet the required performance standards (e.g., from the EU drinking water directive), leading to unreliable data [18].
Solution:
- Benchmark Current Performance: Participate in interlaboratory comparison or proficiency testing (PT) schemes to determine your current Coefficient of Variation (CV%) for the problematic analytes [18].
- Compare with Requirements: Contrast your laboratory's CV% with the maximum standard uncertainty permitted by the relevant regulation (see Table 1 for examples) [18].
- Identify Problematic Analytes: Focus improvement efforts on analytes where the average CV% in PT schemes consistently exceeds the maximum required standard uncertainty (e.g., Bromate, Cyanide, many pesticides, and PAHs) [18].
- Method Optimization: For identified problematic analytes, investigate and optimize the analytical method. This may involve using more specific instrumentation, improving sample preparation, or implementing stricter internal quality control measures [18].
Frequently Asked Questions (FAQs)
FAQ 1: What is the recommended framework for classifying sequence variants in a clinical research setting? The five-tier system developed by the International Society for Gastrointestinal Hereditary Tumours (InSiGHT) is a robust model. This system, adapted from the IARC guidelines, classifies variants as: Pathogenic (Class 5), Likely Pathogenic (Class 4), Uncertain (Class 3), Likely Not Pathogenic (Class 2), and Not Pathogenic (Class 1) [17].
FAQ 2: How can we ensure our variant classifications are consistent with other laboratories? Consistency is achieved through collaboration and data sharing. Submit your variant data to public locus-specific databases (LSDBs) and participate in initiatives like the InSiGHT Variant Interpretation Committee, which provides expert-reviewed, consensus classifications for public use [17].
FAQ 3: For which types of analytical compounds is it most challenging to meet interlaboratory consistency requirements? Data from drinking water analysis shows that consistency is most difficult to achieve for certain trace elements (e.g., Aluminum, Arsenic, Lead), organic trace compounds (e.g., Benzene), and a significant majority of pesticides and their metabolites [18].
FAQ 4: What are the direct clinical implications of each variant classification class? The classification directly guides patient management:
- Classes 5 & 4: Predictive testing of at-risk relatives is recommended, and those who test positive should follow full high-risk surveillance guidelines [17].
- Class 3 (Uncertain): Predictive testing is not offered, and surveillance should be based on family history and other risk factors [17].
- Classes 1 & 2: Manage the patient and family as if "no mutation detected" for the specific disorder. Predictive testing is not recommended [17].
Data Presentation
Table 1: Example Interlaboratory Comparison Data for Drinking Water Analysis
This table, derived from proficiency testing (PT) results, compares the required maximum standard uncertainty from the EU drinking water directive with the average CV% observed in PT schemes, indicating where analytical quality consistently meets or fails requirements [18].
| Analyte Category | Example Analyte | Maximum Standard Uncertainty (%) | Average CV% in PT | Requirements Fulfilled? |
|---|---|---|---|---|
| Major Components | Nitrate | 8 | 4 | Yes [18] |
| Manganese | 8 | 9 | No [18] | |
| Trace Elements | Arsenic | 8 | 13 | No [18] |
| Copper | 8 | 5 | Yes [18] | |
| Volatile Organic Compounds | Benzene | 19 | 26 | No [18] |
| Chloroform | 19 | 15 | Yes [18] | |
| Pesticides | Atrazine | 19 | 17 | Yes [18] |
| Dimethoate | 19 | 42 | No [18] |
Experimental Protocols
Protocol 1: Standardized Variant Classification Using the Five-Tier InSiGHT System
Objective: To consistently classify sequence variants in Mendelian disease genes for clinical reporting and research.
Methodology:
- Variant Curation: Collect all sequence variants and standardize nomenclature. Exclude somatic variants if the focus is on constitutional (germline) disease [17].
- Committee Review (Delphi Consensus Process): A multidisciplinary committee reviews all available evidence for each variant [17].
- Evidence Integration: Evaluate and weigh multiple lines of evidence, including:
- Population Data: Frequency in control populations.
- Computational/Predictive Data: In silico prediction scores.
- Segregation Data: Co-segregation with disease in families.
- Functional Data: Results from validated functional assays (e.g., for mismatch repair genes, this includes in vivo and in vitro assays of protein function) [17].
- Classification Assignment: Assign a final class (1-5) based on predefined criteria that translate the combined evidence into a posterior probability of pathogenicity [17].
- Data Dissemination: Update the locus-specific database with the consensus classification and all supporting evidence to ensure transparency [17].
Protocol 2: Assessing Analytical Performance via Interlaboratory Comparison
Objective: To evaluate a laboratory's analytical performance and measurement uncertainty against external standards and peers.
Methodology:
- Proficiency Testing (PT): Participate in a recognized PT scheme where all laboratories analyze the same homogenized sample material [18].
- Data Analysis by Organizer: The PT provider calculates robust summary statistics (e.g., using the Q-method as described in ISO/TS 20612:2007) from all participant results to determine the assigned value and the observed interlaboratory CV% [18].
- Performance Evaluation: The individual laboratory's result is compared to the assigned value. The standard uncertainty for the analyte is also evaluated against the required maximum standard uncertainty from the relevant directive (e.g., EU drinking water directive) [18].
- Trend Analysis: Monitor the laboratory's performance and the overall PT CV% over time to identify persistent issues with specific analytes and to gauge improvements in the field's analytical quality [18].
Mandatory Visualizations
Five-Tier Variant Interpretation Workflow
Interlaboratory Comparison Evaluation Logic
The Scientist's Toolkit
Table 2: Research Reagent Solutions for Variant Interpretation
| Item | Function/Brief Explanation |
|---|---|
| Locus-Specific Database (LSDB) | A curated repository (e.g., InSiGHT database hosted on LOVD) that aggregates variant data, evidence, and classifications from multiple sources, serving as the primary resource for consensus [17]. |
| Validated Functional Assays | In vivo or in vitro tests (e.g., for mismatch repair deficiency) that provide direct evidence of a variant's effect on protein function, a critical line of evidence for classification [17]. |
| Microattribution Identifiers (ORCID) | A system (e.g., Open Researcher and Contributor ID) used to provide credit for unpublished data submissions, incentivizing data sharing to resolve variants of uncertain significance [17]. |
| Proficiency Testing (PT) Scheme | An interlaboratory comparison program that provides homogeneous samples for analysis, allowing a lab to benchmark its analytical performance and uncertainty against peers and standards [18]. |
| Standardized Nomenclature (e.g., HGVS) | Guidelines for uniformly describing sequence variants, which is a foundational step to avoid confusion and ensure all data for a given variant is aggregated correctly [17]. |
Implementing Standardized Frameworks: ACMG/AMP Guidelines and Gene-Specific Specifications
FAQs on Implementation and Troubleshooting
FAQ 1: Our laboratory encounters frequent discordant variant classifications. What is the root cause of this inconsistency, and what evidence supports it?
A primary cause of discordance is the variable application and weighting of the 28 ACMG/AMP criteria across different laboratories. A key study evaluating nine clinical laboratories revealed that while the ACMG/AMP framework was compatible with internal methods (79% concordance), the initial inter-laboratory concordance using the ACMG/AMP guidelines was only 34% [19]. This significant variation stemmed from differences in how curators interpreted and applied the same evidence criteria to the same variants. After structured consensus discussions, concordance improved to 71%, demonstrating that increased specification and collaborative review are critical for improving consistency [19].
FAQ 2: How can we standardize the use of computational prediction tools to prevent poor-performing methods from overruling better ones?
A common pitfall is the guideline recommendation to use multiple prediction tools that must agree. This practice can allow lower-performing tools to negatively impact the overall assessment [20]. Benchmarking studies show that different computational predictors can disagree on a substantial portion of variants, with one analysis of nearly 60,000 variants showing 10%–45% of predictions were contradictory depending on the tools chosen [20].
Troubleshooting Protocol:
- Tool Selection: Do not rely solely on tools listed in older guidelines. Perform a systematic literature review to identify tools with state-of-the-art performance in independent benchmark studies like CAGI challenges [20].
- Avoid Redundancy: Select a limited number (e.g., one or two) of high-performance predictors that are not based on identical principles or training data to avoid bias [20].
- Expert Oversight: The choice of tools should be made by personnel with bioinformatics expertise who can interpret benchmarking results and understand the underlying methodologies [20].
FAQ 3: How should we adjust population frequency thresholds (BA1/BS1) for genes associated with different diseases?
The ACMG/AMP guideline provides a generic BA1 threshold (allele frequency >5%), but this is an order of magnitude higher than necessary for many rare Mendelian disorders [21]. Blindly applying this threshold can lead to misclassifying pathogenic variants as benign in high-penetrance genes.
Troubleshooting Protocol:
- Calculate Gene-Specific Thresholds: Use the following formula to establish a more accurate, gene-specific threshold for your disease of interest [21]:
- Threshold = (Allowable Affected Frequency) / (Square root of Disease Prevalence)
- A conservative "Allowable Affected Frequency" is often set at 0.02 (2%).
- Use Filtering Allele Frequency (FAF): When querying population databases like gnomAD, utilize the provided Filtering Allele Frequency (FAF). This value represents the highest true population allele frequency for which the upper bound of the 95% confidence interval is still less than the variant’s observed count, functioning as a conservative lower-bound estimate [21].
- Consider Dataset Ascertainment: Understand the composition of your population dataset. For example, gnomAD primarily comprises adults, making it unlikely to contain many individuals with severe pediatric diseases, but it should not be considered a collection of "healthy controls" for adult-onset conditions [21].
FAQ 4: The "Pathogenic" and "Benign" classification seems like a false dichotomy for some genes. How can we handle genes where variants confer risk rather than cause disease?
This is a recognized limitation of the original guidelines, which were optimized for highly penetrant Mendelian disorders. For complex diseases or genes where variants act as risk factors, the five-tier system can be insufficient [22].
Expanded Framework Protocol: To address this continuum of variant effects, consider an adapted framework based on the gene's role in disease causation [22]:
- For "Disease-Causing Genes" (e.g.,
PRSS1in hereditary pancreatitis), use the standard five categories. - For "Disease-Predisposing Genes" (e.g.,
CFTR,CTRCin chronic pancreatitis), replace "Pathogenic" and "Likely Pathogenic" with the categories "Predisposing" and "Likely Predisposing" to more accurately reflect their role in disease risk [22]. This creates a five-category system better suited for multifactorial conditions.
Key Experimental Protocols for Addressing Interlaboratory Differences
Protocol 1: Conducting a Variant Classification Concordance Study
This protocol is based on the methodology used by the Clinical Sequencing Exploratory Research (CSER) consortium to quantify inter-laboratory differences [19].
1. Variant Selection and Distribution:
- Select a set of variants (e.g., ~100) that span all five classification categories (Pathogenic, Likely Pathogenic, VUS, Likely Benign, Benign).
- Include a mix of variant types (missense, nonsense, indels) and difficulties.
- Designate a subset of variants (e.g., 9) to be interpreted by all participating laboratories to measure core concordance.
- Distribute the remaining variants so that each is interpreted by at least three different laboratories.
2. Independent Curation:
- Each laboratory classifies each variant using the ACMG/AMP guidelines.
- Laboratories must document every ACMG/AMP criterion (e.g., PM1, PS3, BP4) invoked for their decision.
3. Data Analysis:
- Calculate Concordance: Use statistical measures like Krippendorff’s alpha to quantify the level of agreement between laboratories, both on the final classification and the individual criteria used [19].
- Identify Discrepancies: Analyze variants with discordant classifications to pinpoint which criteria were applied differently.
4. Consensus Resolution:
- Convene discussions among laboratories to review discordant variants.
- Use the ACMG/AMP framework as a common language to debate the evidence and reach a consensus classification.
- Document the rationale for resolving each discrepancy to create a knowledge base for future guidance.
Protocol 2: Implementing a Quantitative Bayesian Framework
The ClinGen Sequence Variant Interpretation (SVI) Working Group has developed a quantitative framework to refine the strength of ACMG/AMP criteria [21].
1. Assign Quantitative Odds:
- Use the SVI-estimated odds of pathogenicity for each evidence strength level [21]:
- Supporting (PP3, BP4): 2.08:1
- Moderate (PM1, PM4): 4.33:1
- Strong (PS2, PS3, BS2): 18.7:1
- Very Strong (PVS1): 350:1
2. Evaluate Functional Assays:
- For a functional assay used to apply the PS3 criterion, calculate the probability that a variant with a "damaging" result is truly pathogenic.
- If assessment indicates that ~90% of variants with damaging calls are truly pathogenic, the odds are ~9:1. Compare this to the quantitative scale: 9:1 odds fall between "Moderate" (4.33:1) and "Strong" (18.7:1), suggesting a "Moderate" strength level is appropriate rather than a "Strong" one [21]. This provides a data-driven method for assigning criterion strength.
Quantitative Data on Variant Interpretation Consistency
Table 1: Inter-laboratory Concordance in Variant Classification (CSER Study)
| Metric | Initial Concordance | Post-Consensus Concordance | Number of Laboratories |
|---|---|---|---|
| ACMG/AMP Guidelines | 34% | 71% | 9 [19] |
| Laboratories' Internal Methods | Information Missing | 79% ( Intra-lab ACMG vs. Internal Method) | 9 [19] |
Table 2: Quantitative Odds of Pathogenicity for Evidence Strength Levels (ClinGen SVI)
| Evidence Strength | Odds of Pathogenicity | Approximate Probability of Pathogenicity | Example ACMG/AMP Criteria |
|---|---|---|---|
| Supporting | 2.08 : 1 | 67% | PP3, BP4 |
| Moderate | 4.33 : 1 | 81% | PM1, PM4 |
| Strong | 18.7 : 1 | 95% | PS3, BS2 |
| Very Strong | 350 : 1 | >99% | PVS1 |
Table 3: Concordance in Application of Individual ACMG/AMP Criteria
| Study Description | Finding on Concordance | Context |
|---|---|---|
| Comparison of ACMG criteria selection across 36 labs [23] | Average concordance rate for individual criteria was 46% (range 27%-72%) | Highlights the subjective interpretation of when to apply specific criteria codes. |
Visualizing the Framework and Specification Process
ACMG/AMP Specification Workflow: This diagram outlines the process for creating gene or disease-specific specifications for the ACMG/AMP guidelines, moving from the generic rules to a calibrated and quantitative output [21].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Resources for ACMG/AMP Variant Interpretation
| Resource Name | Type | Primary Function in Variant Interpretation |
|---|---|---|
| Genome Aggregation Database (gnomAD) [21] | Population Database | Provides allele frequency data across diverse populations to assess variant rarity using metrics like Filtering Allele Frequency (FAF). |
| ClinVar [24] | Clinical Database | A public archive of reports on variant classifications and supporting evidence from multiple clinical and research laboratories. |
| Critical Assessment of Genome Interpretation (CAGI) [20] | Benchmarking Platform | Independent challenges that evaluate the prediction performance of computational tools, aiding in the selection of best-performing methods. |
| ClinGen Sequence Variant Interpretation (SVI) WG [21] | Expert Consortium | Provides updated recommendations, specifications, and a quantitative framework for applying and evolving the ACMG/AMP guidelines. |
| ClinGen Variant Curation Expert Panels (VCEPs) [21] | Expert Committees | Develop and publish disease-specific specifications for the ACMG/AMP guidelines for specific gene-disease pairs (e.g., MYH7, FBN1). |
| dbNSFP / VarCards [20] | Prediction Aggregator | Databases that aggregate pre-computed predictions from numerous computational tools, streamlining the in-silico evidence collection process. |
| ACMG/AMP Pathogenicity Calculator [19] | Software Tool | Automated tools that help ensure evidence codes are combined according to the ACMG/AMP rules, reducing calculation errors during classification. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary sources of interlaboratory differences in classifying variants in PALB2 and ATM? Interlaboratory differences primarily arise from the interpretation of Variants of Uncertain Significance (VUS). The core challenge is the application of general guidelines, like the ACMG/AMP framework, to genes with unique functional characteristics without gene-specific refinement. For example, in PALB2, a missense variant in the coiled-coil domain may disrupt the BRCA1 interaction, while a variant in the WD40 domain may cause protein instability [25]. Without functional assays to distinguish these mechanisms, one lab might classify a variant based on computational predictions (e.g., PP3 evidence), while another might weight the lack of family segregation data (PP1) differently, leading to discrepant classifications [26].
FAQ 2: How can functional assays reduce classification discrepancies for PALB2 VUS? Functional assays provide objective, experimental evidence on a variant's impact on protein function, which is a strong (PS3) or supporting (PS1) evidence type in the ACMG/AMP framework. For instance, a cDNA-based complementation assay for PALB2 can directly test a variant's ability to rescue DNA repair defects in Palb2 knockout mouse embryonic stem cells [25]. Results from such semi high-throughput assays can definitively categorize VUS as either functionally normal or damaging. This replaces subjective interpretations with standardized, quantitative data—such as a variant's performance in Homologous Recombination (HR) efficiency relative to wild-type controls—directly addressing a major source of interlaboratory disagreement [25] [27].
FAQ 3: What are the key risk estimates for guiding the classification of pathogenic variants in PALB2 and ATM? Accurate risk estimates are crucial for calibrating the clinical significance of a variant. The table below summarizes key risk estimates from a large multicenter case-control study [28].
Table 1: Key Cancer Risk Estimates for Selected PALB2 and ATM Variants
| Gene | Variant | Cancer Type | Population | Odds Ratio (95% CI) | p-value |
|---|---|---|---|---|---|
| PALB2 | c.1592delT | Breast | European women | 3.44 (1.39 to 8.52) | 7.1×10â»âµ |
| PALB2 | c.3113G>A | Breast | European women | 4.21 (1.84 to 9.60) | 6.9×10â»â¸ |
| ATM | c.7271T>G | Breast | European women | 11.0 (1.42 to 85.7) | 0.0012 |
| CHEK2 | c.538C>T | Breast | European women | 1.33 (1.05 to 1.67) | ≤0.017 |
FAQ 4: Why is the ATM c.7271T>G variant classified as high-risk despite its wide confidence interval? The ATM c.7271T>G variant is classified as high-risk due to a very high point estimate (OR=11.0) and a statistically significant p-value (p=0.0012), even though its 95% confidence interval is wide (1.42 to 85.7) [28]. The wide interval reflects the variant's rarity, which makes precise risk estimation challenging with even large sample sizes. Such a significant result strongly indicates pathogenicity. Consistent with ACMG/AMP guidelines, this statistical evidence, combined with other data like its predicted loss-of-function mechanism, supports a Pathogenic or Likely Pathogenic classification, prompting clinical actionability despite the statistical uncertainty [28] [26].
Troubleshooting Guides
Issue 1: Inconsistent Classification of Missense VUS in PALB2
Problem: Different laboratories are assigning conflicting clinical classifications (e.g., VUS vs. Likely Pathogenic) for the same missense variant in PALB2.
Solution: Implement a standardized functional assay workflow to generate objective, gene-specific evidence.
Step-by-Step Protocol: Functional Complementation Assay for PALB2 VUS [25]
Cell Line Preparation:
- Establish a mouse embryonic stem (mES) cell line with a knockout (KO) of the endogenous Palb2 gene. A Trp53 KO background can be used to facilitate cell viability [25].
- Integrate a DNA repair reporter system, such as the DR-GFP reporter, into this cell line to measure Homologous Recombination (HR) efficiency.
Vector Construction and Stable Expression:
- Clone the human PALB2 cDNA wild-type sequence into a Recombination-Mediated Cassette Exchange (RMCE) vector.
- Use site-directed mutagenesis to introduce the specific VUS into the PALB2 cDNA.
- Perform FlpO-mediated, site-specific integration of the wild-type and VUS PALB2 constructs into the Rosa26 locus of the Trp53KO/Palb2KO mES cells. Use a pooled population of neomycin-resistant clones to control for expression level variability.
Functional Analysis:
- HR Efficiency Assay: Transfert the DR-GFP reporter cells with an I-SceI endonuclease plasmid to induce a site-specific double-strand break. Measure HR efficiency by quantifying the percentage of GFP-positive cells using flow cytometry 48-72 hours post-transfection.
- Additional Read-Outs (Optional):
- PARP Inhibitor Sensitivity: Expose cells to a PARP inhibitor (e.g., Olaparib) and perform a cell viability assay (e.g., CellTiter-Glo) after 5-7 days. Pathogenic variants confer hypersensitivity.
- G2/M Checkpoint Analysis: Irradiate cells and analyze the cell cycle profile via flow cytometry to assess checkpoint proficiency.
Data Interpretation and Classification:
- Normalize all HR efficiency results to the wild-type PALB2 control (set at 100%).
- Variants that rescue HR efficiency to levels statistically indistinguishable from wild-type (e.g., >70% of wild-type function) provide strong evidence for a benign impact (BS3 evidence).
- Variants that consistently fail to rescue the HR defect (e.g., <30% of wild-type function) provide strong evidence for a pathogenic impact (PS3 evidence).
This workflow for the functional complementation assay can be visualized as follows:
Issue 2: Translating Somatic Tumor Sequencing Findings to Germline Action
Problem: A potential pathogenic variant is identified in a tumor (somatic) sequencing report for ATM, and the clinical team is unsure whether to initiate germline genetic testing.
Solution: Follow a systematic workflow to evaluate the likelihood of a germline origin.
Table 2: Research Reagent Solutions for Variant Interpretation
| Reagent / Tool | Function in Research | Application in Troubleshooting |
|---|---|---|
| DR-GFP Reporter | Measures repair of I-SceI-induced double-strand breaks via homologous recombination. | Quantifies functional impact of VUS in PALB2, ATM, and other HR genes [25]. |
| RMCE System | Enables site-specific, single-copy integration of cDNA constructs at a defined genomic locus. | Ensures consistent, comparable expression levels of wild-type and variant constructs, reducing experimental noise [25]. |
| Saturation Genome Editing (SGE) | CRISPR-Cas9-based method to test all possible SNVs in a gene domain for functional impact. | Generates high-throughput functional data for missense variants, resolving VUS at scale [27]. |
| VarCall Bayesian Model | A hierarchical model that assigns pathogenicity probability from functional scores. | Provides a standardized, statistical framework for classifying variants from MAVE data, reducing subjective interpretation [27]. |
| ClinVar Database | Public archive of reports on genomic variants and their relationship to phenotype. | Serves as a benchmark for comparing internal variant classifications with the wider community to identify discrepancies [26]. |
Evaluate the Somatic Variant:
- Check Variant Allele Frequency (VAF): A VAF around 50% (or 100% in a loss-of-heterozygosity region) in tumor DNA is suggestive of a germline origin. However, VAF can be confounded by tumor ploidy and purity.
- Review the Gene and Variant: ATM is an established hereditary cancer gene. Note the variant's type (e.g., nonsense, frameshift, missense) and its ACMG classification in ClinVar.
- Assess Tumor Type Concordance: Confirm that the cancer type (e.g., breast, pancreatic) is associated with germline ATM mutations [29] [30].
Make a Clinical Decision:
- If the somatic variant is a known Pathogenic/Likely Pathogenic (P/LP) ATM variant: Refer the patient to a genetic counselor for discussion of confirmatory germline testing. This finding meets criteria for germline follow-up per recent guidelines [30].
- If the somatic variant is a VUS: The decision is more complex. If the variant has a high VAF and is a protein-truncating type, or if functional data (e.g., from a MAVE study) suggests pathogenicity, a genetics referral is still warranted. If evidence is weak, it may be prudent to monitor the variant's classification in databases.
Coordinate Germline Confirmation:
- Order germline genetic testing using a clinical-grade panel on a blood or saliva sample. A negative germline result confirms the variant was somatic-only, while a positive result identifies a heritable mutation with implications for the patient's therapy and family members [29].
The logical pathway for resolving a somatic finding can be summarized in this diagram:
FAQs: Resolving Common Data Interpretation Challenges
1. We observe conflicting variant classifications between databases. Which source should be prioritized for clinical decision-making?
Conflicting classifications between ClinVar and HGMD are common, with studies showing that ClinVar generally has a lower false-positive rate [31]. For clinical decision-making, prioritize variants with multiple submitters in ClinVar and those reviewed by ClinGen Expert Panels (displaying 2-4 stars in ClinVar's review status) [31] [26]. These represent consensus interpretations with higher confidence. HGMD entries, while useful for initial screening, should be corroborated with other evidence as they can imply disease burdens orders of magnitude higher than expected when tested against population data [31].
2. A variant is listed as disease-causing in HGMD but is present at a high frequency in gnomAD. Is this a misclassification?
This is a classic indicator of potential misclassification. A variant too common to cause a rare disease provides strong evidence for a benign interpretation [31] [24]. Use the following ACMG/AMP evidence codes:
- BS1 (Benign Strong): Allele frequency is greater than expected for the disorder [32] [26].
- PM2 (Pathogenic Moderate): Absent from or at extremely low frequency in population databases (supports pathogenicity) [32] [26].
Calculate whether the gnomAD allele frequency exceeds the expected disease prevalence. Reclassify the variant accordingly, giving greater weight to the population frequency evidence.
3. How can we systematically reduce Variants of Uncertain Significance (VUS) in our pipeline?
High VUS rates, particularly in underrepresented populations, remain a major challenge [26]. Implement these strategies:
- Family segregation studies: Check if the variant co-segregates with disease in affected family members (ACMG/AMP code PP1) [26].
- Functional data integration: Incorporate validated functional studies (PS3/BS3 evidence) [26].
- Regular reanalysis: Schedule periodic reinterpretation (every 1-2 years) as new evidence emerges [24] [26].
- Data sharing: Contribute resolved cases to ClinVar to benefit the community [9].
4. Why does the same variant receive different classifications from different clinical laboratories in ClinVar?
Interlaboratory discordance affects approximately 10-40% of variant classifications [9]. Major causes include:
- Different thresholds for evidence: Laboratories may set different allele frequency cutoffs for ACMG/AMP criteria like PM2 [9].
- Asymmetric information access: Laboratories may have access to different in-house data or literature [9].
- Professional judgment differences: Application of criteria requires some expert judgment, leading to variability [9].
- Gene-specific knowledge: Genes with more exons, longer transcripts, and association with multiple distinct conditions show higher rates of conflicting interpretations [33].
Troubleshooting Guide: Addressing Technical and Interpretation Challenges
| Challenge | Root Cause | Solution |
|---|---|---|
| High False Positive Rate | Using outdated classifications; over-reliance on single evidence sources [31]. | Cross-reference HGMD “DM†variants with ClinVar and gnomAD; remove common variants (MAF > disease prevalence) [31]. |
| Population Bias in Interpretation | Underrepresentation of non-European ancestry in genomic databases [31] [26]. | Use ancestry-specific frequency filters in gnomAD; consult population-matched databases if available [31]. |
| Inconsistent ACMG/AMP Application | Subjectivity in interpreting criteria like PM2 (“extremely low frequencyâ€) [9]. | Adopt ClinGen SVI specifications; use quantitative pathogenicity calculators [34]. |
| Variant Classification Drift | Knowledge evolution causing reclassification over time [31] [24]. | Implement automated re-evaluation protocols; track ClinVar review status updates [24]. |
| Handling Conflicting Evidence | Weighing pathogenic and benign evidence for the same variant [35]. | Use modified ACMG/AMP rules from ClinGen; prioritize functional evidence and segregation data [26]. |
Step-by-Step Protocol: Resolving Conflicting Variant Interpretations
Objective: Systematically resolve conflicts when ClinVar and HGMD provide discordant variant classifications.
Materials:
- Computer with internet access
- Variant identifier (RS number, HGVS nomenclature)
- Access to: ClinVar, gnomAD, HGMD (professional license recommended), UCSC Genome Browser
Procedure:
Initial Assessment
- Query the variant in both ClinVar and HGMD simultaneously
- Record all classification assertions and review status
- Note the number of submitters in ClinVar and their assertion criteria
Evidence Collection
- Population Frequency: Extract allele frequencies from gnomAD, noting ancestry-specific distributions
- Computational Predictions: Run multiple in silico tools (SIFT, PolyPhen-2, CADD)
- Functional Evidence: Search for published functional studies in PubMed
- Segregation Data: Check for family studies in ClinVar submissions or literature
ACMG/AMP Criteria Application
- Use the ClinGen Pathogenicity Calculator or similar tool
- Apply disease-specific guidelines if available from ClinGen Expert Panels
- Document each evidence code with strength and direction
Adjudication
- Give greater weight to evidence from multiple independent submitters
- Prioritize functional evidence over computational predictions
- Consider disease mechanism and gene constraint (LOEUF scores from gnomAD)
Documentation and Submission
- Document the final classification and supporting evidence
- Consider submitting novel interpretations to ClinVar
- Update internal databases with resolution date and criteria
Troubleshooting:
- If evidence remains truly conflicting, maintain VUS classification
- For novel variants without functional data, pursue targeted functional assays
- For common conflicts in specific genes, consult relevant ClinGen Expert Panel
Systematic workflow for resolving conflicting variant interpretations between databases
| Resource | Function & Application | Key Features |
|---|---|---|
| gnomAD Browser | Population frequency reference for assessing variant rarity and common polymorphisms [24]. | Ancestry-specific allele frequencies; constraint scores (LOEUF); quality metrics [36]. |
| ClinVar | Public archive of variant interpretations with clinical significance [31]. | Multiple submitter data; review status stars; linked to ClinGen expert panels [37]. |
| HGMD Professional | Catalog of published disease-associated variants from literature [31]. | Extensive literature curation; mutation type annotation; disease associations. |
| ClinGen Allele Registry | Variant normalization and identifier mapping across databases [34]. | Canonical identifiers; cross-database querying; API access. |
| Variant Effect Predictor (VEP) | Functional consequence prediction of variants [33]. | Multiple algorithm integration; regulatory region annotation; plugin architecture. |
| ClinGen Pathogenicity Calculator | Standardized ACMG/AMP criteria implementation [34]. | Quantitative evidence scoring; ClinGen SVI guidelines; documentation generation. |
Key Methodologies from Recent Studies
Quantifying Database Accuracy Improvements Over Time
A 2023 study in Genome Medicine established a methodology to track variant classification accuracy by using inborn errors of metabolism (IEMs) as a model system [31]. Researchers analyzed samples from the 1000 Genomes Project to identify individuals with genotypes classified as pathogenic in ClinVar and HGMD archives. Due to the rarity of IEMs, nearly all such classified pathogenic genotypes in this generally healthy population indicate likely variant misclassification [31]. The key metrics included:
- False-positive rate calculation: Comparing implied disease burden from database classifications against known disease prevalence
- Temporal analysis: Tracking reclassification rates over 6 years across different ancestry groups
- Ancestry bias assessment: Measuring differences in misclassification rates across global populations
Analysis of Conflicting Interpretations in ClinVar
A 2024 study systematically analyzed variants with conflicting interpretations of pathogenicity (COIs) in ClinVar [33]. The methodology included:
- Data extraction: ClinVar VCF files from April 2018 to April 2024, filtered for variants with COI status
- Gene enrichment analysis: Hypergeometric testing to identify genes with statistically significant COI enrichment
- Functional characterization: Gene Ontology and Human Phenotype Ontology analysis of COI-enriched genes
- Variant consequence analysis: Integration with gnomAD allele frequencies and Variant Effect Predictor annotations
This study found that 5.7% of variants have conflicting interpretations, with 78% of clinically relevant genes harboring such variants [33].
Leveraging Clinical Decision Support Software for Standardized Workflows
Clinical Decision Support (CDS) systems are designed to provide healthcare professionals with evidence-based information at the point of care. By integrating various inputs such as electronic medical record (EMR) data, clinical databases, external guidelines, and prediction algorithms, CDS delivers timely guidance to optimize decision-making [38]. For genomic medicine, where interlaboratory inconsistencies in variant interpretation present significant challenges, CDS offers a promising pathway toward standardization. These inconsistencies, with reported rates of 10-40% across laboratories, can lead to discrepant genetic diagnoses and affect clinical management decisions [9]. Implementing standardized CDS tools within variant interpretation workflows can help mitigate these discrepancies by ensuring uniform application of classification criteria across different laboratories and research settings.
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our research team encounters inconsistent variant classifications when using different clinical databases. How can CDS help resolve this?
A: CDS systems can integrate multiple clinical databases through standardized application programming interfaces (APIs) like FHIR (Fast Healthcare Interoperability Resources). This provides a unified interface that reconciles differences according to predefined rules based on the 2015 ACMG/AMP guidelines. Ensure your CDS is configured to prioritize sources with the highest evidence levels and flag conflicts for manual review. Implementation of CDS Hooks allows for real-time consultation of external applications during EMR workflows, providing actionable guidance when discrepancies are detected [38].
Q2: We observe different interpretations of the ACMG/AMP PM2 criterion (allele frequency) across laboratories. How can CDS address this variability?
A: This is a common challenge as the ACMG/AMP guideline states "extremely low frequency" without specifying universal thresholds. Laboratories may set different allele frequency cutoffs (0.1%, 0.5%, or 1%). A CDS solution can standardize this by:
- Implementing configurable, institution-wide thresholds for population frequency data
- Applying natural language processing to latest literature for updated evidence
- Providing transparent documentation of criteria application for audit trails
- Regular synchronization with population databases like gnomAD to ensure current allele frequency data [9]
Q3: Our CDS system generates alerts that disrupt researcher workflow. How can we maintain support without creating interference?
A: This relates to the "Five Rights" of CDS framework - delivering the right information, to the right person, in the right format, through the right channel, at the right time [38]. To optimize:
- Implement passive alerts instead of interruptive pop-ups for non-critical information
- Use CDS Hooks to provide contextual suggestions without blocking workflow
- Customize alert thresholds based on variant criticality and research context
- Provide options for researchers to defer or customize notification preferences
Q4: How can we ensure our CDS system adapts to evolving variant classification evidence?
A: Configure your CDS for continuous learning through:
- Automated periodic reanalysis of variant classifications
- Integration with systems that monitor newly published literature
- Implementation of machine learning algorithms that incorporate updated clinical correlations
- Establishing protocols for manual review when automated systems detect significant evidence changes Regular synchronization with public databases like ClinVar ensures your system incorporates the latest community interpretations [9].
Troubleshooting Common Technical Issues
Problem: CDS tools fail to integrate with existing laboratory information systems.
- Solution: Verify compatibility with interoperability standards like SMART on FHIR, which establishes secure authentication and sharing of EMR context. Work with IT specialists to ensure proper API configuration and data mapping between systems [38].
Problem: Discrepancies between computational predictions and functional evidence in variant assessment.
- Solution: Implement a tiered evidence weighting system within your CDS that clearly distinguishes between computational predictions and functional validation data. Use the CDS to flag conflicts for prioritized expert review rather than automated resolution [9].
Problem: Researcher non-adherence to CDS recommendations.
- Solution: Investigate whether the issue stems from alert fatigue, lack of trust, or workflow disruption. Optimize using the "Five Rights" framework, provide education on the evidence base supporting recommendations, and solicit researcher feedback for system improvements [38].
Quantitative Data on Variant Interpretation Consistency
Reported Rates of Interlaboratory Variant Interpretation Inconsistency
Table 1: Summary of Variant Interpretation Inconsistency Rates from Published Studies
| Study | Number of Variants | Disease Context | Five-Tier Inconsistency Rate | Three-Tier Inconsistency Rate | Medically Significant Difference Rate |
|---|---|---|---|---|---|
| Amendola et al., 2016 [9] | 99 | Unlimited | 66% → 29%* | 41% → 14%* | 22% → 5%* |
| Garber et al., 2016 [9] | 293 | Neuromuscular disorders, skeletal dysplasia, short stature | 56.7% | 33% | Not Mentioned |
| Furqan et al., 2017 [9] | 112 | Hypertrophic cardiomyopathy | Not Mentioned | 20.5% → 10.7%* | 17% → 9.8%* |
| Harrison et al., 2017 [9] | 6,169 | Unlimited | Not Mentioned | 11.7% → 8.3%* | 5% → 2%* |
| Amendola et al., 2020 [9] | 158 | 59 genes reported by accidental discovery | 16% | 29.8% → 10.8%* | 11% → 4.4%* |
Rates shown before and after reanalysis, data sharing, and interlaboratory discussion
Criticality Assessment Color-Coding System for Variant Interpretation
Table 2: Standardized Color-Coding for Assessing Variant Interpretation Criticality
| Color Zone | State of Criticality | Definition | Priority of Action |
|---|---|---|---|
| Green [39] | Safe/Secure | Any hazards are controlled, latent, or undetectable | Proceed while avoiding known hazards |
| Amber [39] | Non-routine/Uncertain | Abnormality detected but unclear if represents imminent threat | Increase vigilance to trap and check deviations; proceed with caution |
| Red [39] | Critical | Clear and present danger identified, may already be causing harm | Make decisions to mitigate the threat |
| Blue [39] | Complex Critical | System unstable, harm evident and compounding | Immediate rescue action needed to avert irreversible outcome |
| Dark Grey [39] | Aftermath/Resolution | Situation has stabilized or progressed to final outcome | Reflect and learn from the outcome |
Experimental Protocols for Standardization
Protocol 1: Implementing CDS for Variant Interpretation Consistency
Objective: To integrate Clinical Decision Support tools into variant interpretation workflows to minimize interlaboratory discrepancies.
Materials:
- Laboratory Information Management System (LIMS) with API capabilities
- CDS software with FHIR compatibility
- ACMG/AMP classification criteria database
- Curated variant database (ClinVar, lab-specific database)
- High-performance computing resources for analysis
Methodology:
- System Configuration:
- Map existing variant classification workflows to identify critical decision points
- Configure CDS to provide ACMG/AMP criteria suggestions at each decision point
- Establish standardized evidence thresholds for population frequency (PM2), computational predictions (PP3/BP4), and functional data (PS3/BS3)
Integration:
- Implement SMART on FHIR protocols for EMR integration
- Configure CDS Hooks for non-interruptive decision support during variant review
- Establish bidirectional data exchange between CDS and laboratory systems
Validation:
- Retrospectively analyze historical variant classifications with and without CDS
- Measure consistency rates between multiple reviewers using the same variants
- Compare classification outcomes with external references (ClinVar submissions)
Continuous Improvement:
Protocol 2: Resolving Discordant Variant Interpretations
Objective: To establish a standardized process for resolving variant interpretation discrepancies between laboratories.
Materials:
- CDS system with collaboration capabilities
- Secure data sharing platform
- Variant visualization tools
- Evidence curation dashboard
Methodology:
- Discrepancy Identification:
- Configure CDS to flag variants with conflicting interpretations between internal and external databases
- Implement automated alerts when new evidence contradicts existing classifications
Evidence Review:
- Use CDS to compile all available evidence for the discordant variant
- Apply standardized weighting to different evidence types following ACMG/AMP guidelines
- Utilize CDS-facilitated virtual review sessions with multiple laboratories
Consensus Building:
- Implement structured deliberation protocols within the CDS
- Document reasoning for classification decisions comprehensively
- Establish escalation pathways for unresolvable discrepancies
Resolution Implementation:
- Update classification in all connected systems simultaneously
- Document resolution rationale for future reference
- Communicate changes to all relevant stakeholders [9]
Workflow Visualizations
CDS-Enhanced Variant Interpretation Workflow: This diagram illustrates the integration of Clinical Decision Support systems into the variant interpretation process, highlighting critical points where standardization reduces interlaboratory discrepancies.
CDS Standardization Mechanism: This visualization shows how Clinical Decision Support systems serve as a central standardization engine, processing diverse evidence sources to deliver consistent variant interpretations across different researchers and laboratories.
Research Reagent Solutions
Essential Tools for CDS-Enhanced Variant Interpretation Research
Table 3: Key Research Reagents and Solutions for Standardized Variant Interpretation
| Reagent/Solution | Function | Implementation Considerations |
|---|---|---|
| SMART on FHIR API [38] | Enables secure integration of external applications with EMR systems | Requires compatibility with existing laboratory information systems; ensures secure authentication and data sharing |
| CDS Hooks [38] | Provides contextual suggestions at point of decision in workflow | Configurable to avoid alert fatigue; can be tailored to specific variant interpretation scenarios |
| ACMG/AMP Criteria Module [9] | Standardized application of variant classification criteria | Requires regular updates to reflect evolving guidelines; configurable thresholds for specific gene-disease pairs |
| Interlaboratory Data Sharing Platform [9] | Facilitates consensus building through shared evidence review | Must address privacy and regulatory concerns; enables real-time collaboration on discordant variants |
| Machine Learning Algorithms [40] | Enhances prediction of variant pathogenicity through pattern recognition | Dependent on high-quality training data; requires validation against established classification methods |
| Color-Coded Criticality Assessment [39] | Visual signaling of interpretation confidence and clinical urgency | Standardized color semantics across laboratories; accommodates color vision deficiencies |
| Automated Reanalysis System [9] | Periodically reassesses variants based on new evidence | Configurable reanalysis triggers; manages version control of classification changes |
Resolving Discordance: Practical Strategies for Laboratories and Researchers
In genomic medicine and drug development, inconsistent variant interpretation between laboratories poses a significant challenge to research reproducibility and patient care. A 2024 international survey of genetics professionals found that functional data are the single largest contributor to conflicting variant interpretations between clinical laboratories [41]. This technical support center provides actionable troubleshooting guides and experimental protocols to standardize data sharing practices and resolve these discrepancies through collaborative reassessment.
Frequently Asked Questions (FAQs)
FAQ 1: Why is shared functional data critical for resolving variants of uncertain significance (VUS)? Experimental functional data can provide the evidence needed to reclassify a significant portion of VUS. When available, functional evidence has been shown to enable the reclassification of 15–75% of VUS for commonly tested tumor suppressor genes like BRCA1, TP53, PTEN, and MSH2 [41].
FAQ 2: What are the most common barriers to using shared functional data? A 2024 survey revealed that 91% of genetics professionals consider insufficient quality metrics or confidence in data accuracy as a major barrier. Additionally, 67% reported that functional data for variants of interest is rarely or never available when needed [41].
FAQ 3: How can we ensure the ethical reuse of shared clinical trial data? A established framework recommends six core principles: (1) Ensure a governance framework, (2) Assess compatibility for data use, (3) Ensure a fair balance of interests, (4) Apply a sound scientific approach, (5) Protect privacy and confidentiality, and (6) Demonstrate oversight and accountability [42].
FAQ 4: What are the benefits of data sharing for the clinical trial enterprise? Responsible data sharing can maximize the value of existing research, potentially reduce the size of control groups in future trials (allowing more patients to receive active therapy), and improve the safety of clinical trials by providing a deeper knowledge base [43] [42].
FAQ 5: What technical challenges exist with data generated for long-read sequencing? Interlaboratory studies highlight challenges in extracting high-molecular-weight (HMW) DNA, which is crucial for long-read sequencing. DNA yield and purity can vary significantly between laboratories and extraction methods, impacting downstream sequencing performance and structural variant analysis [44].
Troubleshooting Guides
Guide 1: Troubleshooting Conflicting Functional Evidence
Problem: Your interpretation of a variant's pathogenicity conflicts with data from another laboratory.
Solution: Follow this systematic workflow to investigate and resolve the discrepancy.
Detailed Steps:
Audit Internal Data & Methodology
- Review all quality control metrics for your functional assay. In a recent survey, 94% of respondents noted that better access to primary functional data and standardized interpretation would significantly improve usage [41].
- Document your analysis pipeline version and parameters, as updates can impact results. A systematic reanalysis of clinical genome sequencing data using an updated pipeline and software allowed researchers to find diagnoses for 14 more patients in a 350-sample cohort [45].
Compare External Data Sources
- Request the complete methodology from the other laboratory, including assay conditions and quality metrics.
- Verify whether both laboratories are using common data standards, such as those being developed for the Trusted Exchange Framework and Common Agreement (TEFCA) to improve interoperability [46] [47].
Reanalyze Using Standardized Tools
- Utilize the latest bioinformatic software and pipelines. Advanced tools are essential for efficiently interrogating medically relevant but challenging genomic regions [45].
- Apply established guidelines from organizations like the Clinical Genome Resource (ClinGen) Sequence Variant Interpretation (SVI) Working Group for translating functional data into evidence for variant classification [41].
Initiate Collaborative Reassessment
- Engage in direct dialogue with the other laboratory for a joint data review.
- Reach consensus on the interpretation based on all available evidence, and submit the updated classification to public databases like ClinVar.
Guide 2: Troubleshooting Data Usability and Exchange
Problem: You are unable to effectively use or share datasets due to format inconsistencies and interoperability issues.
Solution: Implement strategies to improve data quality and standardize exchange protocols.
Key Solutions:
- Adopt Common Data Standards: Utilize implementation guides, such as the CDISC-SEND standard for nonclinical data, to structure datasets and avoid common errors that regulatory bodies like the FDA frequently observe [48].
- Implement Data Usability Frameworks: Leverage resources like The Sequoia Project's Data Usability Workgroup Implementation Guide to drive semantic interoperability and improve data quality [46].
- Establish Clear Governance: Create a strong governance framework that details the scope of acceptable secondary research activities and designates experts to evaluate the risk profile of these activities [42].
Experimental Protocols for Collaborative Research
Protocol 1: Standardized DNA Extraction for Long-Read Sequencing
Purpose: To minimize interlaboratory variation in DNA extraction, ensuring optimal yield and quality for long-read sequencing and structural variant analysis.
Summary of Key Findings from an Interlaboratory Study (2025):
The table below summarizes the performance of four common HMW DNA extraction methods, based on an interlaboratory study using the GM21886 reference cell line [44].
| Extraction Method | Median Yield (µg/million cells) | Key Strength | Notable Limitation |
|---|---|---|---|
| Nanobind (NB) | ~1.9 | Most consistent yield; highest proportion of ultra-long reads (>100 kb) | Higher variability in DNA purity (A260/230 ratios) |
| Fire Monkey (FM) | ~1.7 | Highest N50 read length values; low within-sample heterogeneity | Lower proportion of ultra-long reads |
| Genomic-tip (GT) | ~1.3 | Highest sequencing yields | Lower DNA fragment size linkage at long distances (150 kb) |
| Puregene (PG) | ~0.9 | - | Highest variability in yield and purity; inconsistent HMW DNA peak |
Methodology Details [44]:
- Sample Input: 3.3 - 5 million cryopreserved cells from a reference cell line (e.g., GM21886) with known chromosomal alterations.
- QC Step 1 - DNA Purity: Assess using UV spectrophotometry (A260/280 and A260/230 ratios). Target A260/280 ≥ 1.8 and A260/230 ≥ 2.0.
- QC Step 2 - DNA Fragment Size:
- Pulsed-Field Gel Electrophoresis (PFGE): Confirm the majority of the DNA smear exceeds 50 kb.
- Digital PCR Linkage Assay: A more quantitative method. Measures the percentage of linked molecules at set genomic distances (e.g., 33, 100, 150 kb). Linkage at 150 kb is a key indicator for ultra-long read sequencing success.
- Sequencing: After size selection, proceed with standard library preparation for long-read sequencing platforms (e.g., Oxford Nanopore Technologies).
Protocol 2: Reassessment of Variant Classifications Using Shared Data
Purpose: To systematically reanalyze a cohort of genetic variants using updated pipelines and shared data resources to increase diagnostic yield.
Methodology (Based on a 2025 Study) [45]:
- Cohort Selection: Identify a cohort of unsolved cases or variants of uncertain significance (e.g., 350 samples from a previous clinical trial).
- Data Re-processing: Re-run the entire raw dataset through an updated bioinformatic pipeline (e.g., the DRAGEN pipeline from the cited study).
- Reinterpretation: Reinterpret variants using advanced software (e.g., Emedgene software from the cited study) and the latest available evidence from shared databases.
- Validation: Confirm new diagnostic findings using orthogonal methods when necessary.
The table below lists key reagents, tools, and resources essential for experiments in data sharing and variant reassessment.
| Item Name | Function / Application | Example / Source |
|---|---|---|
| Reference Cell Line | Provides a controlled source of DNA with known variants for method validation and interlaboratory studies. | GM21886 [44] |
| HMW DNA Extraction Kits | Isolate high-quality, long-strand DNA essential for long-read sequencing and structural variant detection. | Nanobind, Fire Monkey, Genomic-tip, Puregene [44] |
| Bioinformatic Pipelines | Analyze sequencing data; updated versions can uncover new diagnoses from existing data. | DRAGEN pipeline, Emedgene software [45] |
| Data Usability Implementation Guide | Provides community-driven standards to improve the quality and consistency of shared health data. | The Sequoia Project Data Usability Workgroup Implementation Guide (DUIG) [46] |
| Public Data Repositories | Enable data sharing, provide access to large-scale datasets for analysis, and facilitate reinterpretation. | ClinVar, UK Biobank, All of Us, Project Data Sphere [49] [41] |
| Privacy & Governance Framework | Guides the ethical and compliant secondary use of clinical data for research. | TransCelerate Biopharma's "A Privacy Framework For Secondary Research" [42] |
Troubleshooting Guides and FAQs
The Pitfalls of Majority Voting
Q: What is the "majority vote" pitfall and why is it a problem for my research?
A: The "majority vote" pitfall occurs when researchers use the same underlying data or highly correlated prediction tools multiple times and simply count the results, treating computational tools as black boxes. This approach is scientifically unsound because it can create a false consensus. As noted in computational methodology literature, this practice, along with incomplete reporting of methods and extending methods beyond their intended purpose, can significantly affect the interpretation of your results [50] [51]. This is particularly problematic in variant interpretation research where interlaboratory differences already pose significant challenges.
Q: How does the majority vote problem specifically impact interlaboratory studies?
A: In interlaboratory studies, consistency is crucial for reliable results. The GEMINI study, which compared genomic sequencing to targeted gene panels, highlighted that variant interpretation differences between laboratories contributed to a 43% discrepancy in molecular diagnostic yield [52]. When individual laboratories additionally employ flawed majority vote approaches internally, these interlaboratory differences are further amplified, making it difficult to compare or replicate findings across different research centers.
Troubleshooting Common Computational Workflow Issues
Q: My computational workflow produces inconsistent results across different runs. How can I stabilize it?
A: Inconsistent results often stem from three main issues: dependency management, inadequate version control, or insufficient computational resource specification. To stabilize your workflows:
- Containerize Dependencies: Use Docker or Singularity containers to package all tools and dependencies, ensuring consistent execution environments across runs [53].
- Implement Semantic Versioning: Use clear version numbers (MAJOR.MINOR.PATCH) for all tools and workflows to maintain control over changes [53].
- Document Computational Requirements: Explicitly specify memory, CPU, and storage requirements in your workflow documentation to prevent resource-related inconsistencies [54].
Follow the FAIR Principles for computational workflows to enhance reliability: ensure your workflows are Findable, Accessible, Interoperable, and Reusable [54]. This includes using persistent identifiers (DOIs), standard workflow languages (CWL, WDL, Nextflow), and comprehensive metadata.
Q: How can I properly validate my computational predictions without relying on problematic majority voting?
A: Instead of simple majority voting, implement these validation strategies:
- Use Orthogonal Validation Methods: Employ different algorithmic approaches that don't share underlying training data or methodological assumptions.
- Implement Tiered Evidence Systems: Classify predictions based on strength of supporting evidence rather than simple vote counts.
- Incorporate Experimental Validation: Where possible, include wet-lab confirmation for critical predictions.
- Consult Independent Method Assessments: Use performance evaluations from authoritative sources rather than selecting tools on unscientific grounds [50].
Table: Comparison of Problematic vs. Recommended Validation Approaches
| Approach | Methodology | Risk of False Consensus | Suitable for Interlab Studies |
|---|---|---|---|
| Majority Vote | Counting results from correlated tools | High | No |
| Orthogonal Validation | Using fundamentally different methods | Low | Yes |
| Tiered Evidence System | Weighting evidence by quality and source | Medium | Yes |
| Experimental Confirmation | Wet-lab validation of predictions | Lowest | Yes |
Addressing Interlaboratory Variability
Q: What practical steps can my laboratory take to minimize interlaboratory differences in variant interpretation?
A: The GEMINI study provides crucial insights into reducing interlaboratory differences [52]. Implement these evidence-based strategies:
- Standardize Interpretation Frameworks: Adopt common variant interpretation guidelines across all laboratories in your consortium.
- Implement Regular Proficiency Testing: Participate in interlaboratory comparison schemes similar to those used in other medical fields [55] [56].
- Conduct Joint Data Analysis Sessions: Regularly review discordant variants with partner laboratories to understand interpretation differences.
Q: How significant are interlaboratory differences in genetic testing, and what impact do they have on patient care?
A: The GEMINI study demonstrated that interlaboratory variant interpretation differences are substantial and clinically meaningful. This multicenter study found that variant interpretation by laboratories differed by 43%, which directly affected molecular diagnostic yields [52]. These differences potentially impact clinical management decisions, as the study found that changes in clinical care affected 19% of participants, and 76% of clinicians viewed genomic testing as useful or very useful in clinical decision-making [52].
Table: Interlaboratory Variability in Proficiency Testing - Example from DOAC Measurement
| Parameter | Dabigatran | Rivaroxaban | Apixaban | International Normalized Ratio |
|---|---|---|---|---|
| Coefficient of Variation | 8.7% | 8.4% | 10.3% | 11.4% |
| Responsive Test | Thrombin Time | Prothrombin Time | Prothrombin Time | N/A |
| Test Responsiveness | High for APTT | High for PT | Moderate for PT | N/A |
Data adapted from interlaboratory proficiency testing of direct oral anticoagulants, demonstrating that dedicated tests show relatively small interlaboratory variability comparable to established international standards [55].
Technical Implementation Guide
Q: What are the essential technical requirements for making our computational workflows robust and shareable across laboratories?
A: To ensure your computational workflows can be reliably used across different laboratory environments:
- Expose All Parameters via Command Line: Ensure every option is configurable at runtime through command-line arguments, not hard-coded values or configuration files [53].
- Use Standard Input/Output Streams: Implement conventional stdin, stdout, and stderr streams for data transfer between workflow components [53].
- Create Comprehensive Documentation: Include both high-level project documentation and detailed interface-level documentation describing all inputs, outputs, data types, and units [53].
- Implement Proper Version Control: Use Git with a consistent branching model (Git Flow or GitHub Flow) and host on collaborative platforms like GitHub or GitLab [53].
Q: How can we effectively package and distribute our computational tools to ensure consistent results across different laboratory environments?
A: Distribution consistency requires a multi-layered approach:
- Use Package Managers: Distribute tools through standard package managers like Conda, Pip, or Yum to handle dependency management automatically [53].
- Containerize Complex Dependencies: Create Docker or Singularity containers that encapsulate all software dependencies [53].
- Provide Clear Installation Scripts: Automate installation processes to minimize manual configuration errors.
- Offer Test Datasets: Include sample inputs and expected outputs to verify correct installation and functioning [54].
Research Reagent Solutions: Essential Materials for Computational Workflows
Table: Key Computational Research Reagents for Variant Interpretation Studies
| Research Reagent | Function/Purpose | Implementation Examples |
|---|---|---|
| Workflow Management Systems | Coordinates execution of multiple computational components | Nextflow, Snakemake, Galaxy, CWL [54] |
| Containerization Platforms | Encapsulates dependencies for consistent execution | Docker, Singularity, OCI-compliant containers [53] |
| Version Control Systems | Tracks changes and enables collaboration | Git, Subversion, GitHub, GitLab [53] |
| Provenance Tracking Tools | Records data lineage and execution history | Workflow-native logging, specialized provenance frameworks [54] |
| Metadata Standards | Enables discovery and reuse of workflows | Schema.org, Bioschemas, domain-specific ontologies [54] |
| Workflow Registries | FAIR-compliant platforms for sharing workflows | WorkflowHub, Dockstore [54] |
Experimental Protocols for Standardization
Protocol: Interlaboratory Proficiency Testing for Computational Methods
Based on established proficiency testing frameworks used in medical laboratories [55] [56]:
- Sample Distribution: Central organizers prepare and distribute standardized test datasets to all participating laboratories.
- Blinded Analysis: Laboratories analyze the test datasets using their routine computational pipelines without special treatment or excessive testing.
- Result Submission: Participants submit results to the organizing body by predetermined deadlines.
- Statistical Analysis: The organizing body calculates performance scores (e.g., z-scores) for each laboratory and test parameter.
- Confidential Reporting: Individual laboratories receive confidential reports comparing their performance to the group aggregate, identified only by code numbers.
Key Considerations: Test datasets should represent realistic scenarios while containing specific challenges to properly evaluate performance. As with wet-lab proficiency testing, "the goal is to get a good impression of the quality of the normal routine performance of the laboratory" without extra efforts to achieve perfect scores [56].
Protocol: Implementing FAIR Principles for Computational Workflows
Based on established FAIR guidelines for computational workflows [54]:
Findability Implementation:
- Assign persistent identifiers (DOIs) to workflows via repositories like Zenodo or WorkflowHub
- Register workflows in searchable registries like Dockstore
- Use rich metadata including author information, creation dates, and scientific applications
Accessibility Assurance:
- Host workflows on platforms using standard HTTPS protocols
- Ensure metadata remains accessible even if workflow execution becomes temporarily unavailable
- Implement standard authentication when necessary
Interoperability Enhancement:
- Use formal workflow languages (CWL, WDL, Nextflow)
- Employ standardized vocabularies and ontologies (EDAM for bioinformatics)
- Ensure components read/write data in domain-standard formats
Reusability Optimization:
- Provide comprehensive documentation including README files, installation instructions, and example data
- Apply clear open-source licenses (Apache 2.0, MIT, GPL)
- Maintain detailed provenance information including version history and development process
Workflow Diagrams
Diagram 1: Problematic vs. Recommended Computational Approaches
Diagram 2: FAIR Computational Workflow Implementation
Diagram 3: Interlaboratory Standardization Process
Refining Population Frequency Thresholds and Phenotype Correlations
Frequently Asked Questions (FAQs)
Q1: Why is the conventional genome-wide significance threshold of 5 × 10â»â¸ not always sufficient? The conventional threshold was established based on assumptions about the human genome's linkage disequilibrium (LD) structure that may not hold across diverse populations or when analyzing rare variants. African populations, which exhibit greater genetic diversity and shorter LD blocks, often require more stringent thresholds, while the standard threshold can be overly conservative for some European and Asian populations, especially for common variants [57].
Q2: How does Minor Allele Frequency (MAF) influence the choice of a significance threshold? The effective number of independent tests in a genome-wide association study (GWAS) increases when rarer variants (lower MAF) are included in the analysis. This necessitates the use of more stringent significance thresholds to control the family-wise error rate (FWER) effectively. Using MAF-specific thresholds provides a more accurate framework than a single, fixed value [57].
Q3: What is a key first step in ensuring consistent variant interpretation across different labs? A critical first step is implementing rigorous Data Collection and Quality Assessment. This involves gathering comprehensive patient and family history information and utilizing automated quality assurance systems to monitor sequencing data in real-time. Adherence to quality standards like ISO 13485 is also crucial for maintaining credibility and data integrity [24].
Q4: Which databases are essential for assessing the clinical relevance of a genetic variant? Two widely used public databases are:
- ClinVar: A curated public archive that reports the relationships between genetic variants and their clinical significance (e.g., pathogenic, benign) [24].
- gnomAD (Genome Aggregation Database): A resource that aggregates population-level frequency data from large-scale sequencing projects, which helps determine if a variant is too common in the general population to be the cause of a rare disorder [24].
Q5: How can computational tools aid in variant interpretation? Computational prediction tools provide an initial assessment of a variant's potential impact by analyzing how amino acid changes might affect protein structure or function. While not definitive on their own, they are valuable for prioritizing variants for further, more rigorous investigation [24].
Troubleshooting Common Experimental Challenges
Issue 1: Inconsistent variant significance calls between laboratories working on the same population cohort.
- Potential Cause: Differences in the application of multiple testing corrections, especially if the populations have diverse LD structures.
- Solution: Implement population-specific and MAF-specific significance thresholds.
Protocol: The Li-Ji Method for Calculating Effective Number of Independent Tests [57]
- Partition the Genome: Use a tool like LDetect to divide the genome into natural LD blocks based on population-specific recombination patterns.
- Generate LD Matrices: For each LD block, calculate the linkage disequilibrium (correlation) matrix between genetic variants.
- Apply the Li-Ji Formula: Perform eigenvalue decomposition on the correlation matrix. The effective number of independent tests (M~eff~) is calculated as: M~eff~ = Σ f(|λ~i~|) Where the function f is defined as: Here, λ~i~ are the eigenvalues, I is an indicator function, and ⌊x⌋ is the floor of x.
- Aggregate and Calculate: Sum the M~eff~ from all blocks to get a genome-wide total. The Bonferroni-adjusted significance threshold is then 0.05 / M~eff~.
Comparison of Multiple Testing Correction Methods:
Method Brief Description Key Advantage Li-Ji Method Calculates effective number of tests using eigenvalues of the LD correlation matrix [57]. More accurate as it accounts for both strong and weak correlations without overcounting [57]. SimpleM Method Uses principal components to estimate the number of tests needed to explain 99.5% of variance [57]. Computationally tractable for large-scale analyses [57].
Issue 2: A variant is classified as a Variant of Uncertain Significance (VUS) and its clinical impact is unclear.
- Potential Cause: Insufficient evidence from population frequency, computational predictions, or functional data to classify the variant as pathogenic or benign.
- Solution: Follow a structured framework that integrates multiple lines of evidence.
- Protocol: A Step-by-Step Workflow for VUS Interpretation [24]
- Check Population Frequency: Query gnomAD. A variant with a frequency higher than the disease prevalence in the general population is likely benign. Be aware of population-specific frequencies [24].
- Interrogate Clinical Databases: Search ClinVar and CIViC for existing classifications or literature on the variant [24].
- Run Computational Predictions: Use in silico tools to predict the variant's effect on protein function (e.g., SIFT, PolyPhen-2) and splicing [24].
- Correlate Genotype with Phenotype: Assess if the variant segregates with the disease in family studies and if it matches the known inheritance pattern (e.g., autosomal dominant, recessive) [24].
- Seek Functional Validation: If evidence remains inconclusive, perform or request functional assays (e.g., measuring protein stability, enzymatic activity, or splicing efficiency) to validate the biological impact [24].
Issue 3: Discrepancy in phenotype correlation for a known pathogenic variant.
- Potential Cause: The presence of putative modifier genes or other genetic factors that can alter the disease expression and severity.
- Solution: Acknowledge and investigate the potential for modifier genes when establishing genotype-phenotype correlations, as their influence can explain clinical heterogeneity among patients carrying the same primary mutation [58].
Experimental Protocols & Data Presentation
Table 1: Genome-Wide Significance Thresholds by Population and MAF [57] This table summarizes how the Bonferroni-adjusted significance threshold becomes more stringent for populations with greater genetic diversity and when including rarer variants.
| Population | Common Variants (MAF ≥ 0.05) | Threshold with Rare Variants | Key Genetic Reason |
|---|---|---|---|
| African | More stringent than 5 × 10â»â¸ | Even more stringent than 5 × 10â»â¸ | Shorter LD blocks, greater genetic diversity [57]. |
| European | Somewhat lower than 5 × 10â»â¸ | More stringent than 5 × 10â»â¸ | Longer LD blocks due to historical bottlenecks [57]. |
| Asian | Somewhat lower than 5 × 10â»â¸ | More stringent than 5 × 10â»â¸ | LD structure somewhat similar to European populations [57]. |
Table 2: Research Reagent Solutions for Variant Interpretation A list of key databases, tools, and standards essential for consistent and reliable variant interpretation.
| Item Name | Type | Primary Function in Research |
|---|---|---|
| LDetect Database | Software/Tool | Partitions the genome into population-specific LD blocks for accurate calculation of independent tests [57]. |
| ClinVar Database | Database | Public archive of reported variant-disease associations and clinical significance [24]. |
| gnomAD Database | Database | Provides allele frequency data across diverse populations to filter out common polymorphisms [24]. |
| ACMG-AMP Guidelines | Standard | Provides a standardized framework for classifying variants into pathogenicity categories (Pathogenic, VUS, Benign) [24]. |
| omnomicsNGS Platform | Software/Tool | Integrates and automates variant interpretation workflows, from raw sequencing data to annotated, prioritized variants [24]. |
Methodology and Workflow Visualizations
Variant Interpretation Workflow
Multiple Testing Correction Concept
Systematic Re-evaluation and Management of Variants of Uncertain Significance (VUS)
Variants of Uncertain Significance (VUS) represent one of the most significant challenges in clinical genomics today. With the widespread adoption of next-generation sequencing (NGS), laboratories are identifying an increasing number of genetic variants whose clinical significance remains unknown. More than 70% of all unique variants in the ClinVar database are currently classified as VUS, creating substantial barriers to clinical decision-making and potentially resulting in unnecessary clinical recommendations, follow-up testing, and procedures [59].
The VUS problem is particularly pronounced in underrepresented populations, where the lack of diverse genetic reference data leads to disproportionately higher VUS rates. This disparity creates significant inequities in the diagnostic power of genetic testing across different ethnic groups [26] [60]. Within the context of addressing interlaboratory differences in variant interpretation research, establishing systematic protocols for VUS re-evaluation is essential for improving consistency, reliability, and clinical utility of genetic testing results across different laboratories and populations.
Quantitative Evidence: The Scope and Impact of VUS
VUS Prevalence and Reclassification Rates
Table 1: Documented VUS Prevalence and Reclassification Rates Across Studies
| Study Focus | Cohort Size | VUS Prevalence | Reclassification Rate | Key Findings |
|---|---|---|---|---|
| General Adult Genetics [59] | 5,158 patients | 50.6% of all variant classifications | Not specified | VUS rates varied by >14-fold depending on testing indication and 3-fold by self-reported race |
| HBOC in Middle Eastern Population [60] | 347 patients | 160 VUS detected | 32.5% of VUS reclassified | 4 variants (2.5%) upgraded to Pathogenic/Likely Pathogenic |
| Tumor Suppressor Genes [61] | 145 carriers (128 unique VUS) | Not specified | 31.4% of remaining VUS reclassified as Likely Pathogenic | Highest reclassification in STK11 (88.9%) |
Documentation Gaps and Systemic Challenges
Table 2: Systemic Challenges in VUS Management
| Challenge Category | Documented Issue | Impact |
|---|---|---|
| Reporting Gaps | At least 1.6% of variant classifications in EHRs are outdated compared to ClinVar [59] | 26 instances where lab updated ClinVar but reclassification never communicated to patient |
| Interlaboratory Differences | Professional judgment in ACMG/AMP guideline application leads to discrepancies [26] | Reduced consistency in variant classification across laboratories |
| Population Disparities | VUS rates significantly higher in underrepresented populations [26] [60] | Inequities in diagnostic power of genetic testing |
Methodological Framework: Systematic VUS Re-evaluation
Evidence Integration Workflow for VUS Reclassification
Advanced Classification Using ClinGen PP1/PP4 Criteria
The Clinical Genome Resource (ClinGen) Sequence Variant Interpretation Working Group has developed refined criteria for co-segregation (PP1) and phenotype-specificity (PP4) that significantly enhance VUS reclassification potential. The point-based system transforms ACMG/AMP evidence criteria into quantitative scores [61]:
- Pathogenic (≥10 points)
- Likely Pathogenic (6-9 points)
- VUS (0-5 points)
- Likely Benign (-1 to -6 points)
- Benign (≤-6 points)
Evidence strengths are weighted as:
- Supporting (1 point)
- Moderate (2 points)
- Strong (4 points)
- Very Strong (8 points)
The novel aspect of the ClinGen guidance allows for assigning higher scores based on phenotype specificity criteria when phenotypes are highly specific to the gene of interest. In scenarios of locus homogeneity (where only one gene explains the phenotype), up to five points can be assigned solely from phenotype specificity criteria [61].
Technical Support Center: VUS Re-evaluation FAQs
FAQ 1: How do we establish a systematic VUS re-evaluation protocol in our laboratory?
Answer: Implementing a systematic VUS re-evaluation protocol requires a structured approach:
Develop a Laboratory-Specific SOP: Create standard operating procedures detailing re-evaluation triggers, methods, and documentation requirements. Establish a schedule for periodic re-assessment (e.g., every 3 years) [61].
Utilize Automated Re-evaluation Systems: Implement systems like omnomicsNGS that integrate computational predictions with multi-level data filtering strategies to systematically prioritize variants for re-evaluation [24].
Establish Evidence Integration Protocols: Develop clear protocols for integrating population data (gnomAD), computational predictions (REVEL, SIFT, PolyPhen-2), functional data, and clinical correlations using the ACMG/AMP framework [26] [61].
Implement Quality Assurance Measures: Participate in external quality assessment programs like the European Molecular Genetics Quality Network (EMQN) and Genomics Quality Assessment (GenQA) to ensure consistency and reliability [24].
FAQ 2: What strategies effectively reduce interlaboratory classification discrepancies for VUS?
Answer: Addressing interlaboratory discrepancies requires multiple complementary approaches:
Utilize Expert Panel Guidelines: Adopt disease-specific guidelines developed by ClinGen expert panels, which provide customized criteria for interpreting variants in specific genes like PTEN or TP53 [26].
Implement Quantitative Scoring Systems: Transition to point-based ACMG/AMP classification systems as described by Tavtigian et al. (2018) to reduce subjectivity in variant interpretation [61].
Enhance Data Sharing Practices: Actively contribute to and utilize ClinVar database submissions, paying particular attention to the review status (star rating) to gauge confidence levels in variant interpretations [24] [26].
Standardize Functional Validation: Establish cross-laboratory standardization for functional assays through participation in external quality assessment programs and adherence to international standards like ISO 13485 [24].
FAQ 3: How can we address the disproportionately high VUS rates in underrepresented populations?
Answer: Mitigating population disparities in VUS rates requires targeted strategies:
Implement Population-Specific Assessment: For populations underrepresented in genomic databases (e.g., Middle Eastern, African, Asian), utilize population-specific allele frequency cutoffs and incorporate data from diverse populations when available [60].
Develop Regionally Adapted Classification: Create classification strategies that account for population-specific genetic variations and founder effects that may differ from European-centric databases [60].
Expand Diverse Genomic Data Collection: Prioritize inclusion of underrepresented populations in genomic research and database development to address the current diversity gap in reference datasets [60].
Utilize Family Studies: Implement systematic family studies and segregation analysis to generate population-specific evidence for variant classification [62].
FAQ 4: What evidence types are most impactful for VUS reclassification?
Answer: The most impactful evidence types for VUS reclassification include:
Functional Assays: Well-validated functional studies showing damaging effects (PS3) or no effect (BS3) provide strong evidence. Multiplexed Assays of Variant Effect (MAVEs) can systematically assess variant impact at scale [26].
Phenotype-Genotype Correlations: Highly specific phenotype matches with gene function, especially for genes with locus homogeneity, can provide significant evidence under new ClinGen PP4 criteria [61].
Segregation Analysis: Co-segregation of variant with disease in multiple family members (PP1) following established Bayes point methodologies [61].
Population Data: Absence from population databases (PM2) or high frequency in control populations (BS1) provides critical evidence [26] [61].
FAQ 5: How should laboratories handle communication of VUS reclassifications to patients and providers?
Answer: Effective communication of VUS reclassifications requires:
Establish Clear Re-contact Protocols: Develop systematic approaches for patient re-contact after variant reclassification, considering the points outlined by the American College of Medical Genetics and Genomics (ACMG) in their statement on this topic [59].
Implement EHR Update Procedures: Create systems to ensure electronic health records are updated when variant reclassifications occur, addressing the documented gap where 1.6% of variant classifications in EHRs are outdated [59].
Provide Clinical Decision Support: Work with clinicians to develop clear guidelines on how reclassified variants should impact clinical management, particularly for upgrades to pathogenic/likely pathogenic classifications [62].
Utilize Genetic Counselors: Engage genetic counselors to help bridge the communication gap between the laboratory and the patient, particularly for managing uncertainty and explaining the implications of reclassified variants [26].
Research Reagent Solutions for VUS Re-evaluation
Table 3: Essential Research Reagents and Resources for VUS Investigation
| Resource Category | Specific Tools/Databases | Primary Function | Application in VUS Re-evaluation |
|---|---|---|---|
| Population Databases | gnomAD, 1000 Genomes | Provides allele frequency data across populations | Assess variant rarity; BS1/PM2 evidence application |
| Variant Databases | ClinVar, HGMD | Curated collections of variant-disease associations | Cross-reference prior classifications and evidence |
| Computational Prediction Tools | REVEL, SIFT, PolyPhen-2, CADD, SpliceAI | In silico prediction of variant impact | PP3/BP4 evidence for pathogenicity assessment |
| Functional Assay Platforms | Multiplexed Assays of Variant Effect (MAVEs) | High-throughput functional impact assessment | Generate PS3/BS3 evidence at scale for multiple variants |
| Classification Frameworks | ACMG/AMP Guidelines, ClinGen SVI | Standardized variant classification criteria | Systematic evidence integration and classification |
| Quality Assurance Programs | EMQN, GenQA | External quality assessment | Ensure consistency and reliability of interpretations |
Advanced Reclassification Workflow Using New ClinGen Criteria
This advanced workflow demonstrates how the new ClinGen PP1/PP4 criteria can significantly improve VUS reclassification rates, particularly for tumor suppressor genes with specific phenotypes. The quantitative approach allows for more systematic and transparent variant assessment, directly addressing interlaboratory differences by reducing subjective interpretation elements.
Ensuring Accuracy: Benchmarking Tools and Validating Interpretations
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ 1: Which computational variant effect predictors are currently considered state-of-the-art?
Answer: Based on recent large-scale benchmarking studies, several predictors have demonstrated top-tier performance. A 2024 study published in Genome Biology that evaluated 24 different computational variant effect predictors found that AlphaMissense outperformed all others in inferring human traits based on rare missense variants in both the UK Biobank and All of Us cohorts [63] [64]. Other strong performers included VARITY, ESM-1v, and MPC, which were statistically tied with AlphaMissense for specific gene-trait combinations [63]. It's important to note that predictor performance can vary depending on the specific application and gene involved, so considering a consensus approach from multiple top performers is often recommended [65].
Table: Top-Performing Variant Effect Predictors (2024 Benchmark)
| Predictor Name | Key Strength | Performance Note |
|---|---|---|
| AlphaMissense | Best overall performance across 132/140 gene-trait combinations | Top performer in UK Biobank and All of Us cohorts [63] |
| VARITY | Statistically indistinguishable from AlphaMissense for some traits | Strong clinical correlation [63] |
| ESM-1v | Competitive performance on specific gene-trait combinations | Tied with AlphaMissense for inferring atorvastatin use [63] |
| MPC | Competitive performance on specific gene-trait combinations | Tied with AlphaMissense for some binary phenotypes [63] |
FAQ 2: What are the main causes of interlaboratory differences in variant interpretation, and how can we address them?
Answer: Interlaboratory differences primarily stem from:
- Predictor Selection Bias: Different labs use different VEPs, which have varying performance characteristics [63] [65]. Solution: Establish institutional guidelines for predictor selection based on recent benchmarking studies.
- Data Circularity: Many predictors trained on clinical databases like ClinVar show inflated performance on similar datasets but perform worse on functional data [65]. Solution: Use "population-free" VEPs that aren't trained on clinical labels for more generalizable results.
- Benchmarking Method Flaws: Traditional benchmarks often suffer from circularity where training data contaminates evaluation sets [63]. Solution: Adopt the method used in recent studies that leverage population-level cohorts (UK Biobank, All of Us) not used in predictor training [63] [66].
Troubleshooting Guide: If your lab is experiencing inconsistent variant interpretation:
- Audit your current VEP selection against recent independent benchmarks
- Implement a consensus approach using multiple top-performing predictors with different methodologies
- Validate your pipeline against known gene-trait associations from population biobanks
FAQ 3: What methodology should I use for unbiased benchmarking of computational predictors?
Answer: A robust benchmarking methodology should include:
- Independent Cohort Data: Use population-level cohorts of genotyped and phenotyped participants that have NOT been used in predictor training (e.g., UK Biobank, All of Us) [63].
- Curated Gene-Trait Associations: Begin with a carefully curated set of human gene-trait associations with reported rare-variant burden associations [63].
- Rare Variant Focus: Concentrate on rare missense variants (MAF < 0.1%) as they're more likely to have large phenotypic effects and have sparse clinical annotations [63].
- Appropriate Performance Metrics:
- For binary traits: Use area under the balanced precision-recall curve (AUBPRC)
- For quantitative traits: Use Pearson Correlation Coefficient (PCC) [63]
- Statistical Robustness: Perform bootstrap resampling (e.g., 10k iterations) to estimate uncertainty and calculate false discovery rates for pairwise comparisons [63].
Unbiased Benchmarking Workflow for Variant Effect Predictors
FAQ 4: How do I classify variant effect predictors and what are the implications of each type?
Answer: VEPs can be classified into three categories based on their training data and vulnerability to data circularity:
Table: Variant Effect Predictor Classification and Implications
| Predictor Type | Training Data | Circularity Vulnerability | Performance Characteristics |
|---|---|---|---|
| Clinical Trained | Labeled clinical data from databases (ClinVar, HGMD) | High | Often performs better on clinical datasets than functional ones [65] |
| Population Tuned | Not directly trained with clinical data but may be exposed during tuning | Moderate | Moderate performance across dataset types [65] |
| Population Free | No labeled clinical data or allele frequency features | Low | Most consistent across clinical and functional benchmarks [65] |
Troubleshooting Guide: If concerned about circularity in your predictions:
- Favor "population-free" VEPs for more generalizable results
- Use clinical-trained VEPs only for specific clinical correlation tasks
- Disclose predictor types used when reporting results to enhance reproducibility
FAQ 5: What are the essential guidelines for proper benchmarking methodology?
Answer: Essential benchmarking guidelines include:
- Define Clear Purpose and Scope: Determine if the benchmark is for method development, neutral comparison, or community challenge [66].
- Comprehensive Method Selection: Include all available methods meeting predefined criteria (e.g., freely available, installable without errors) [66].
- Appropriate Dataset Selection: Use both simulated data (with known ground truth) and real experimental data, ensuring they accurately reflect real-world properties [66].
- Avoid Bias: Ensure equal familiarity with all methods or involve original method authors to optimize each method's performance [66].
- Rigorous Evaluation: Use multiple evaluation metrics and consider tradeoffs between different performance aspects rather than relying on single metrics [66].
Answer: Essential research reagents and resources include:
Table: Essential Research Reagent Solutions for VEP Benchmarking
| Resource Name | Type | Function/Purpose |
|---|---|---|
| UK Biobank | Population Cohort | Provides exome-sequenced participants with deep phenotyping for unbiased benchmarking [63] |
| All of Us | Population Cohort | Independent whole-genome sequenced cohort for validation studies [63] |
| ProteinGym | Benchmark Platform | Frequently-updated benchmark with clinical and functional (MAVE) components [65] |
| dbNSFP | Database | Pre-calculated predictions from >40 VEPs for all non-synonymous SNVs [65] |
| VIPdb | Directory | Comprehensive list of >400 VEPs with links and references [65] |
Addressing Interlaboratory Differences in Variant Interpretation
The Role of Functional Assays in Validating Variant Pathogenicity
The widespread adoption of genomic sequencing has revealed millions of genetic variants, most of which are rare and lack clear clinical interpretation. Functional assays provide powerful experimental evidence for determining whether variants disrupt normal gene/protein function, offering critical insights that computational predictions alone cannot provide. These assays constitute some of the strongest types of evidence for classifying variants as pathogenic or benign according to professional guidelines like the ACMG/AMP framework, where well-established functional evidence can provide strong support (PS3/BS3 codes) for variant classification [67].
The challenge of Variants of Uncertain Significance (VUS) is substantial—in clinically actionable genes like BRCA2, approximately 75% of missense variants remain classified as VUS, creating uncertainty for patients and clinicians [68]. Multiplex Assays of Variant Effect (MAVEs) represent a transformative approach that enables simultaneous functional assessment of thousands to millions of variants in a single experiment, moving beyond the limitations of traditional one-at-a-time testing [68]. This technical guide addresses key considerations for implementing functional assays to support variant interpretation while addressing interlaboratory standardization challenges.
Troubleshooting Guides & FAQs
Assay Selection & Validation
Q: How do I determine if my functional assay is suitable for clinical variant interpretation?
A: The Clinical Genome Resource (ClinGen) Sequence Variant Interpretation Working Group recommends a structured four-step framework for evaluating functional assays:
- Define the disease mechanism: Determine whether the gene follows loss-of-function or gain-of-function pathology, as this dictates which assay readouts are clinically relevant [67].
- Evaluate applicability of general assay classes: Consider how closely the assay context (e.g., patient-derived samples, animal models, cellular systems) reflects the biological environment. Assays using patient-derived materials generally provide stronger evidence than in vitro systems [67].
- Evaluate validity of specific assay instances: Assess technical validation parameters including controls, replication, and statistical analysis. The SVI Working Group recommends a minimum of 11 total pathogenic and benign variant controls to establish moderate-level evidence in the absence of rigorous statistical analysis [67].
- Apply evidence to variant interpretation: Determine the appropriate evidence strength (supporting, moderate, strong) based on the assay's validation status and clinical validity [67].
Q: What are the key considerations when developing a MAVE?
A: MAVE development requires careful experimental design to ensure clinical utility:
- Library Design: Comprehensively cover all possible nucleotide substitutions or focus on specific domains with clinical significance [68].
- Selection System: Implement a robust phenotypic selection that accurately reflects the gene's biological function.
- Controls: Include established pathogenic and benign variants throughout the experimental process.
- Replication: Build in technical and biological replicates to assess reproducibility.
- Clinical Correlation: Validate MAVE results against known clinical variants to establish predictive value [68].
Evidence Application & Classification
Q: How should functional evidence be applied within the ACMG/AMP framework?
A: Proper application requires careful consideration of evidence strength:
- PS3/BS3 Codes: Reserve these strong evidence codes for "well-established" assays that have been rigorously validated. Do not apply to preliminary or non-validated assays [67].
- Evidence Strength Tiers: The SVI Working Group has developed a provisional framework for assigning different evidence strength levels (supporting, moderate, strong) based on assay validation metrics [67].
- Statistical Rigor: Assays with comprehensive statistical analysis and larger control variant sets may qualify for higher evidence strength [67].
Common Pitfall: Inconsistent application of PS3/BS3 codes is a major contributor to variant interpretation discordance between laboratories. Always reference gene-specific criteria from ClinGen Variant Curation Expert Panels when available [67].
Q: How do I handle discrepancies between functional data and computational predictions?
A: Functional data typically carries greater weight than in silico predictions in variant classification. However, consider these steps when discrepancies occur:
- Verify Assay Performance: Re-examine your assay's validation metrics and positive/negative controls.
- Check Computational Tool Performance: Be aware that different prediction tools show variable performance across genes and ancestral backgrounds [69] [70].
- Review Disease Mechanism: Ensure the functional assay appropriately reflects the established disease biology.
- Seek Corroborating Evidence: Look for additional evidence types (population data, segregation, etc.) to resolve the discrepancy.
Technical Challenges & Optimization
Q: What strategies can improve reproducibility of functional assays across laboratories?
A: Standardization is key to addressing interlaboratory differences:
- Control Variants: Establish and share a common set of reference variants with known clinical significance.
- Protocol Harmonization: Develop detailed standard operating procedures for assay execution and data analysis.
- Data Sharing: Participate in community resources like ClinGen that aggregate functional evidence across laboratories [71].
- Cross-Validation: Periodically perform interlaboratory comparisons using the same variant sets.
Q: My assay shows intermediate results. How should these be interpreted?
A: Intermediate results present interpretation challenges:
- Dose Effects: For some genes, partial function retention may correlate with milder disease severity.
- Assay Limitations: Determine if intermediate activity reflects true biological effect or technical assay limitations.
- Clinical Correlation: Use clinical data from individuals with the same variant to guide interpretation of intermediate functional results.
- Conservative Classification: When uncertain, maintain VUS classification rather than forcing pathogenic or benign calls.
Experimental Protocols & Methodologies
Multiplex Assays of Variant Effect (MAVE) Workflow
MAVEs enable comprehensive functional assessment of thousands of variants in parallel. The following workflow outlines the key steps for implementing this powerful approach:
Protocol: Deep Mutational Scanning for Missense Variants
- Objective: Systematically measure the functional consequences of all possible amino acid substitutions in a protein domain.
- Applications: Coding variants in disease-associated genes with established molecular functions [68].
Materials:
- Saturation mutagenesis library covering target region
- Appropriate cellular model system (complementing cell lines, yeast, etc.)
- Selection system (drug resistance, growth advantage, FACS sorting)
- Next-generation sequencing platform
- Computational resources for sequence analysis
Methodology:
Library Design & Construction:
- Design oligonucleotides covering all possible nucleotide substitutions in the target region.
- Use array-based synthesis or error-prone PCR to generate variant library.
- Clone library into appropriate expression vector.
Functional Selection:
- Transfer variant library into model system.
- Apply selection pressure relevant to protein function (e.g., ligand binding, enzymatic activity).
- Include control populations (pre-selection) for comparison.
- Perform multiple biological replicates.
Sequencing & Analysis:
- Extract DNA from pre-selection and post-selection populations.
- Amplify target region with barcoded primers for multiplex sequencing.
- Sequence to sufficient depth (>100x coverage per variant).
- Calculate enrichment scores based on variant frequency changes.
Clinical Validation:
- Correlate functional scores with known pathogenic and benign variants.
- Establish classification thresholds based on control variants.
- Validate predictions against clinical databases [68].
Guidelines for Applying Functional Evidence
The ClinGen Sequence Variant Interpretation Working Group has established a structured framework for evaluating functional evidence. This decision pathway helps determine the appropriate evidence strength for variant classification:
Data Analysis & Interpretation
Performance Metrics for Pathogenicity Prediction Tools
When complementing functional data with computational predictions, tool selection should be evidence-based. The table below summarizes performance characteristics of selected prediction tools across different contexts:
Table 1: Performance Characteristics of Pathogenicity Prediction Tools
| Tool Category | Top Performing Tools | Performance Context | Key Considerations |
|---|---|---|---|
| Composite Tools | BayesDel, ClinPred, REVEL, CADD | Generally strong across multiple gene types [69] [72] | BayesDel_addAF identified as most robust for CHD genes [69] |
| AI-Based Tools | AlphaMissense, ESM-1b | Emerging promise with improving accuracy [69] | Rapidly evolving category requiring validation |
| Categorical Tools | SIFT | Most sensitive for CHD variants (93%) [69] | Good for initial screening |
| Ancestry-Specific | MetaSVM, Eigen-raw, MVP | Perform well irrespective of ancestry [70] | Critical for diverse populations |
| African-Specific | MutationTaster, DANN, LRT, GERP-RS | Optimized for African genetic backgrounds [70] | Addresses European bias in genomics |
| European-Specific | MutationAssessor, PROVEAN, LIST-S2, REVEL | Better performance in European backgrounds [70] | Use with caution in non-European populations |
Functional Evidence Criteria Evaluation
Proper application of functional evidence requires systematic evaluation of assay validity. The table below outlines key criteria for assessing functional evidence strength:
Table 2: Evaluating Functional Evidence for ACMG/AMP PS3/BS3 Application
| Evaluation Criteria | Strong Evidence | Moderate Evidence | Supporting Evidence |
|---|---|---|---|
| Control Variants | ≥11 pathogenic AND ≥11 benign variants with concordant results [67] | 5-10 controls of each type with concordant results | <5 controls of each type |
| Statistical Analysis | Comprehensive statistical analysis with established significance thresholds | Basic statistical analysis with p-values | Descriptive analysis only |
| Technical Replication | Multiple independent experiments showing high reproducibility | Limited replication with consistent results | Single experiment |
| Clinical Correlation | Strong correlation with established clinical variants (≥90% concordance) | Moderate correlation (70-89% concordance) | Limited clinical correlation |
| Assay Context | Patient-derived materials or physiological model systems | Engineered cell lines with relevant biology | Non-physiological or in vitro systems |
Research Reagent Solutions
Table 3: Essential Research Reagents for Functional Assays
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Variant Libraries | Saturation mutagenesis libraries, Oligonucleotide pools | Comprehensive coverage of variant space for MAVEs [68] |
| Expression Systems | Mammalian vectors, Yeast systems, Cell-free systems | Delivery and expression of variant libraries in model systems |
| Selection Markers | Drug resistance genes, Fluorescent proteins, Surface tags | Enrichment of functional variants based on phenotypic readouts |
| Control Variants | Known pathogenic/benign variants, Synthetic reference standards | Assay validation and calibration across experiments [67] |
| Sequencing Reagents | Barcoded primers, Library prep kits, Sequencing chemistry | Multiplex analysis of variant populations pre- and post-selection |
| Analysis Tools | Enrichment calculation algorithms, Statistical packages | Quantitative assessment of variant effects from sequencing data |
Functional assays represent an essential component of comprehensive variant interpretation, providing critical evidence that bridges the gap between computational predictions and clinical significance. The standardization of assay validation and evidence application frameworks, particularly through initiatives like ClinGen, is essential for addressing interlaboratory differences and improving consistency in variant classification. As MAVE technologies continue to evolve and generate comprehensive functional maps, their integration with computational approaches and clinical data will be crucial for resolving the interpretation of rare variants and advancing precision medicine.
Comparative Analysis of Database Entries and Cross-Laboratory Classifications
Welcome to the technical support center for researchers working on interlaboratory differences in variant interpretation. This resource provides targeted troubleshooting guides and FAQs to address common experimental challenges you may encounter when comparing database entries or analyzing cross-laboratory classification data. The guidance below is framed within the context of addressing reproducibility challenges in genomic research, particularly for clinical variant interpretation in cancer and hereditary disease genes.
Frequently Asked Questions (FAQs)
Database Selection and Comparison
Q: What are the major challenges when comparing variant classifications across different databases?
A: Research shows substantial disparity in variant classifications exists both across and within publicly accessible databases [73]. One study analyzing BRCA1/BRCA2 variants found that discrepant classifications are not the result of a single outlier but represent widespread disagreement among databases [73]. Key challenges include:
- Inconsistent classification schemes: Different databases may use different evidence-based criteria for pathogenicity assessment
- Data curation methods: Some databases sometimes favor a clinical classification when current best practice guidelines (ACMG/AMP/CAP) would suggest an uncertain classification [73]
- Coverage variation: Approximately one-third of variants with therapeutic implications may be uniquely contained in a single database [74]
Q: Which databases provide the most comprehensive coverage for cancer variant interpretation?
A: Based on a case study of MDS/AML, the VICC (Variant Interpretation for Cancer Consortium) meta-database was the most extensive source of information, featuring 92% of variants with a drug association [74]. However, the study also found that meta-databases lack some variants present in original sources, suggesting researchers should consult multiple resources [74].
Q: How reliable are locus-specific databases (LSDBs) for clinical decision support?
A: While LSDBs have been well-established for research applications, several challenges preclude their wider use in clinical practice [73]. Public databases provide decision support for interpreting variants but there is still a need for manual curation and careful review of evidence-based methodologies for classification [74] [73].
Experimental Design and Cross-Laboratory Comparison
Q: What methodologies can improve reliability in cross-laboratory variant interpretation studies?
A: Implementing structured proficiency testing (PT) and interlaboratory comparison (ILC) schemes is essential [75] [76]. Successful approaches include:
- Using z-score analysis under ISO 13528 to classify laboratory performance [75]
- Establishing uniform testing rules and requirements aligned with EN ISO/IEC 17043 [75]
- Providing all participating laboratories with identical reference materials and testing protocols [75]
- Conducting systematic data analysis of both proficiency tests and method comparison experiments [76]
Q: How significant are interlaboratory differences in practical terms?
A: One study on ceramic tile adhesives found that while 89.5% to 100% of laboratories produced satisfactory results depending on the measurement type, the variability of obtained results was significant enough that manufacturers must consider this in risk analysis [75]. This variability increases the possibility of products failing to meet assessment criteria despite internal validation.
Troubleshooting Guides
Issue: Discrepant Variant Classifications Between Databases
Problem: Your analysis reveals conflicting variant classifications when querying different databases.
Solution: Implement a systematic reconciliation protocol:
Gather Complete Evidence
- Query multiple meta-databases and original sources [74]
- Document the specific evidence cited for each classification
- Note the date of last curation for each entry
Apply Standardized Guidelines
- Use established frameworks like ACMG/AMP/CAP guidelines for reassessment [73]
- Create an evidence-based scoring system for conflicting entries
- Prioritize entries with functional validation data
Resolution Workflow:
Issue: Inconsistent Results in Cross-Laboratory Comparisons
Problem: Your interlaboratory study shows significant variability in variant classification or experimental results.
Solution: Implement quality control measures based on proficiency testing frameworks:
Pre-Study Preparation
Statistical Analysis
- Use z-score analysis to identify outlier laboratories [75]
- Calculate concordance rates across laboratories
- Stratify variants based on classification complexity
Root Cause Investigation:
Database Comparison Metrics
Table 1: Comparison of Open-access Databases for Clinical Variant Interpretation in Cancer (MDS/AML Case Study) [74]
| Database Metric | Value | Context |
|---|---|---|
| Variants with clinical implications | 13% | Of all variants analyzed |
| Therapeutically relevant variants unique to single databases | ~33% | Highlights importance of multi-database queries |
| VICC meta-database coverage | 92% | Of variants with drug associations |
| Missing variants in meta-databases | Present | Some variants absent from meta-databases but in original sources |
Table 2: Concordance Analysis of BRCA1/BRCA2 Variant Classifications Across Five Databases [73]
| Analysis Category | Finding | Research Implication |
|---|---|---|
| Classification agreement | Substantial disparity | Widespread disagreement among databases |
| Database consistency | Not single outlier | Systemic issue across resources |
| Evidence utilization | Variable | Some databases classify as pathogenic when guidelines suggest VUS |
| Clinical readiness | Challenges exist | LSDBs not fully ready for clinical application without curation |
Experimental Protocols
Protocol 1: Cross-Database Variant Comparison Methodology
Purpose: To systematically compare variant classifications across multiple databases and identify discrepancies.
Materials:
- Research Reagent Solutions:
- LSDB Access: Login credentials for relevant locus-specific databases
- Variant Dataset: Curated list of variants to be analyzed
- Classification Mapping Table: Framework for harmonizing different classification schemes
- Evidence Documentation Template: Standardized form for recording supporting evidence
Procedure:
- Dataset Preparation: Compile an unbiased dataset of variants representative of your patient population [73]
- Database Query: Cross-reference each variant against all relevant databases (e.g., BIC, ClinVar, LOVD, UMD, HGMD) [73]
- Classification Mapping: Convert different classification schemes to standardized categories (Pathogenic, Benign, VUS) using predefined criteria [73]
- Discrepancy Identification: Flag variants with conflicting classifications between databases
- Evidence Review: For discrepant variants, examine cited evidence in each database
- Blinded Verification: Perform blinded review by independent reviewers to verify accuracy [73]
Protocol 2: Interlaboratory Proficiency Testing Setup
Purpose: To establish a proficiency testing scheme for assessing cross-laboratory consistency in variant interpretation.
Materials:
- Research Reagent Solutions:
- Reference Variant Set: Curated variants with validated classifications
- Testing Protocol: Standardized methodology document
- Data Collection Platform: Secure system for result submission
- Statistical Analysis Tools: Software for z-score and concordance calculation
Procedure:
- Participant Recruitment: Enroll multiple laboratories performing similar variant interpretation [75]
- Material Distribution: Provide identical reference materials and testing protocols to all participants [75]
- Blinded Analysis: Laboratories analyze provided samples without knowledge of expected results
- Data Collection: Collect results through standardized reporting forms
- Statistical Evaluation: Calculate z-scores and concordance rates according to ISO 13528 [75]
- Feedback Provision: Provide individual and aggregated reports to participants
- Method Refinement: Use results to identify areas for methodological improvement [76]
Research Reagent Solutions
Table 3: Essential Materials for Database Comparison and Interlaboratory Studies
| Reagent/Resource | Function | Application Context |
|---|---|---|
| VICC Meta-Database | Aggregates therapeutic associations | Identifying drug-gable variants across sources [74] |
| ACMG/AMP/CAP Guidelines | Standardized classification framework | Harmonizing variant interpretations across labs [73] |
| Proficiency Testing Materials | Reference samples for validation | Assessing interlaboratory performance [75] |
| Z-Score Analysis Tools | Statistical performance assessment | Quantifying laboratory proficiency [75] |
| Evidence Documentation Templates | Standardized evidence recording | Ensuring consistent data collection across studies |
External Quality Assessment (EQA) and Proficiency Testing for Ongoing Validation
FAQs: Fundamentals of EQA and Proficiency Testing
Q1: What is the core difference between External Quality Assessment (EQA) and Proficiency Testing (PT)?
EQA is a broad system for objectively checking a laboratory's performance using an external agency. Proficiency Testing is a specific method of EQA where laboratories analyze unknown samples provided by an external provider [77]. The terms are often used interchangeably, but PT is a subset of EQA [77].
Q2: Why is EQA/PT participation critical for laboratories involved in variant interpretation research?
EQA/PT is a cornerstone of laboratory quality management. It ensures the accuracy, comparability, and reliability of test results across different institutions [78]. For variant interpretation research, this is vital as it:
- Provides an independent external assessment of your laboratory's current processes [77].
- Allows for peer comparison of biomarker testing, helping to identify and address interlaboratory differences [77].
- Functions as an early warning system for potential problems with tests, processes, or operations [77].
Q3: What are the common types of EQA/PT schemes used for qualitative tests like variant reporting?
Two common approaches are:
- PT with a designated "true value": The PT provider qualifies the reference samples to confirm their biomarker status. Laboratories are evaluated against this known value [77].
- PT with consensus scoring: The PT provider uses a process to determine the consensus score from all participants and designates this as the correct result. This method shows a laboratory's concordance with the wider community but can be problematic if many laboratories report an incorrect result [77].
Q4: Our laboratory is accredited. Is EQA/PT still necessary?
Yes. Participation in EQA/PT is typically required for laboratory accreditation, but the two are complementary and fulfill different functions [77]. Accreditation reflects an assessment of standards at a specific time, whereas EQA/PT is a continuous process that provides ongoing monitoring of performance, making it essential for ongoing validation [77].
Troubleshooting Guides: Addressing Unacceptable EQA/PT Results
Unacceptable EQA/PT results indicate a potential issue with your analytical process. A structured troubleshooting approach is essential. The following workflow outlines a systematic path from initial response to preventive action.
Phase 1: Preliminary Verification
Before investigating complex analytical issues, rule out simple and common errors.
- Action 1.1: Verify Submitted Data: Clerical errors are the most common source of PT failures [79] [80]. Implement a "buddy system" where a second person verifies all data entries against original reports before submission [79].
- Action 1.2: Check Sample Handling: Confirm that all instructions for sample storage, reconstitution, and handling were followed exactly as directed by the PT provider [79]. Assumptions that one event is like the last can lead to mistakes.
Phase 2: Error Type Identification and Investigation
After verification, identify the nature of the error to guide your investigation.
Action 2.1: Investigate Systematic Errors (Consistent Bias): A consistent bias across multiple EQA samples suggests a systematic issue. Key areas to investigate include:
- Reagent Lot Variation: A change in reagent lot can introduce a consistent bias. Check if the error correlates with a new lot number [81].
- Calibration: Review calibration logs and procedures. Verify the calibration curve and its traceability [81].
- Instrument Performance: Check instrument maintenance records, optics, and fluidics for potential issues.
- Assignment of Target Values: Understand how the target value was assigned. If the EQA material is non-commutable, the deviation might be due to a matrix-related bias unique to the EQA sample and not patient samples [81].
Action 2.2: Investigate Random Errors (Isolated Deviation): A large error in a single sample suggests a random, non-reproducible problem. Focus on:
- Pipetting Technique: Inaccurate or imprecise pipetting is a common source of random error. Verify pipette calibration and technician technique.
- Sample Mix-up: Confirm sample identification throughout the testing process.
- Contamination: Check for potential sample-to-sample contamination.
- Data Transcription: Even if the electronic submission was correct, an error might have occurred when transcribing the result from the instrument.
Phase 3: Resolution and Documentation
- Action 3.1: Implement Corrective Actions: Based on your findings, take appropriate action. This may include:
- Retraining staff on specific procedures (e.g., pipetting, data entry).
- Revising standard operating procedures (SOPs).
- Servicing or recalibrating instrumentation.
- Contacting the reagent manufacturer regarding a potential lot issue.
- Action 3.2: Document the Entire Process: Document the unacceptable result, the investigation process, root cause(s) identified, corrective actions taken, and verification of effectiveness. This is a requirement for accreditation standards like ISO 15189 [81] [77].
Essential Materials and Data Interpretation
Key Research Reagent Solutions and Materials
The following table details critical materials used in EQA/PT programs and their functions in the context of ongoing validation.
| Item | Function in EQA/PT |
|---|---|
| Commutable EQA Sample | A control material that behaves identically to native patient samples in all measurement methods. It is the ideal sample type as it provides meaningful information on method trueness and interlaboratory comparability [81]. |
| Non-Commutable EQA Sample | A control material with a matrix that differs from patient samples. It can produce matrix-related biases that do not reflect actual clinical sample performance, limiting the interpretation of results [81]. |
| Reference Measurement Procedure | A higher-order method used to assign a "true" target value to a commutable EQA sample. This allows laboratories to assess the trueness of their measurements [81]. |
| Certified Reference Material | A reference material characterized by a metrologically valid procedure, with an assigned value and associated uncertainty. Used for value transfer to EQA samples when commutability is verified [81]. |
| Peer-Group Consensus Value | An assigned target value calculated as the mean or median of results from laboratories using the same method and instrument. Used when a reference method value is unavailable or the sample is non-commutable [81]. |
Interpreting EQA/PT Performance Scores
Understanding the metrics in your EQA/PT report is crucial for self-assessment. The table below summarizes common performance assessment criteria.
| Metric / Limit Type | Description | Interpretation |
|---|---|---|
| z-Score | Number of standard deviations (SD) the laboratory's result is from the assigned value. Formula: z = (Lab Result - Assigned Value) / SD [81]. | |z| ≤ 2.0: Satisfactory2.0 < |z| < 3.0: Questionable (Warning)|z| ≥ 3.0: Unsatisfactory (Action) [81] |
| Regulatory Limits (e.g., CLIA) | Fixed limits defined by regulatory bodies like the Clinical Laboratory Improvement Amendments (CLIA) [81]. | Identifies laboratories with performance so poor they should not continue testing. These limits are often wider than other types. |
| Clinical Limits | Limits based on what difference might affect clinical decisions or be derived from biological variation data [81]. | The most desirable limits, as they ensure quality based on clinical needs rather than just statistical peer performance. |
Conclusion
Achieving consistent variant interpretation is not merely a technical goal but a fundamental prerequisite for the reliability of genomic medicine in research and clinical practice. The synthesis of strategies outlined—from adopting refined, gene-specific ACMG/AMP guidelines and intelligent data sharing to the careful selection of computational tools and robust validation protocols—provides a clear roadmap toward harmonization. Future progress hinges on global collaboration, the continuous development of functional evidence, and the creation of even more sophisticated bioinformatics platforms. By embracing these approaches, the biomedical community can minimize interpretive noise, enhance diagnostic accuracy, and ultimately accelerate the development of targeted therapies, ensuring that genetic insights translate reliably into improved patient outcomes.
References
- 1. A Framework for Evaluating Diagnostic Discordance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4146522/]
- 2. Discordance in Immunohistochemistry Results in Breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368330/]
- 3. Data sharing to improve concordance in variant interpretation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8523590/]
- 4. Performance of ACMG-AMP Variant-Interpretation ... [https://www.sciencedirect.com/science/article/pii/S0002929716300593]
- 5. Interlaboratory variability of HER2 fluorescence in situ ... [https://diagnosticpathology.biomedcentral.com/articles/10.1186/s13000-024-01588-w]
- 6. Concordance between amyloid PET and CSF biomarkers ... [https://www.nature.com/articles/s41598-025-23759-5]
- 7. 9.4 Guidelines for re-testing and interpretation of ... [https://www.technet-21.org/fr/manual-introduction/chapter-9-laboratory-testing-for-determination-of-population-immune-status/9-4-guidelines-for-re-testing-and-interpretation-of-discordant-and-equivocal-results]
- 8. National quality assurance program using digital ... [http://jpatholtm.org/journal/view.php?doi=10.4132/jptm.2025.06.27]
- 9. Reasons and Resolutions for Inconsistent Variant Interpretation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11919222/]
- 10. Clinical laboratories collaborate to resolve differences in ... [https://www.nature.com/articles/gim201714]
- 11. Assessment of Interlaboratory Variation in the Interpretation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7191323/]
- 12. SPIRIT 2025 statement: updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12035670/]
- 13. Standards [https://www.cdisc.org/standards]
- 14. Study Data Standards Resources [https://www.fda.gov/industry/fda-data-standards-advisory-board/study-data-standards-resources]
- 15. Clinical trial regulations in 2025: navigating the constraints [https://clinicaltrialrisk.org/clinical-trial-design/clinical-trial-regulations-navigating-the-constraints/]
- 16. 10 Clinical Trial Regulatory Changes Coming in 2025 [https://en.ennov.com/blog/clinical-blog/trial-regulatory-changes-coming-2025/]
- 17. Application of a five-tiered scheme for standardized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4294709/]
- 18. sciencedirect.com/topics/earth-and-planetary-sciences/ interlaboratory ... [https://www.sciencedirect.com/topics/earth-and-planetary-sciences/interlaboratory-comparison]
- 19. Performance of ACMG-AMP Variant-Interpretation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4908185/]
- 20. Problems in variation interpretation guidelines and in their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7507483/]
- 21. Overview of specifications to the ACMG/AMP variant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6885382/]
- 22. Expanding ACMG variant classification guidelines into a ... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-022-00407-x]
- 23. Comparison of the ABC and ACMG systems for variant ... [https://www.nature.com/articles/s41431-024-01617-8]
- 24. A Practical Guide to Clinical Variant Interpretation [https://www.euformatics.com/blog-post/a-practical-guide-to-clinical-variant-interpretation]
- 25. Functional analysis of genetic variants in the high-risk ... [https://www.nature.com/articles/s41467-019-13194-2]
- 26. Clinical Variant Interpretation: 5 Easy Tiers [https://lifebit.ai/blog/clinical-variant-interpretation-complete-guide/]
- 27. Functional evaluation and clinical classification of BRCA2 ... [https://www.nature.com/articles/s41586-024-08388-8]
- 28. PALB2, CHEK2 and ATM rare variants and cancer risk [https://pmc.ncbi.nlm.nih.gov/articles/PMC5200636/]
- 29. Practical Considerations and Challenges for Germline ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7735040/]
- 30. New ASCO guidelines for germline genetic testing in ... [https://medicover-genetics.com/new-asco-guidelines-for-germline-genetic-testing-in-patients-with-cancer/]
- 31. ClinVar and HGMD genomic variant classification accuracy ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-023-01199-y]
- 32. Genetic Variant Interpretation Tool [https://www.medschool.umaryland.edu/genetic_variant_interpretation_tool1.html/]
- 33. Major Causes of Conflicting Interpretations of Variant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11355203/]
- 34. The Clinical Genome (ClinGen) Resource [https://www.genome.gov/Funded-Programs-Projects/ClinGen-Clinical-Genome-Resource]
- 35. VCV000313296.15 - ClinVar - NCBI - NIH [https://www.ncbi.nlm.nih.gov/clinvar/variation/313296]
- 36. Resources and tools for rare disease variant interpretation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10206239/]
- 37. Welcome to ClinGen [https://clinicalgenome.org/]
- 38. Understanding Clinical & Data Decision Support Standardization [https://evidence.care/understanding-clinical-decision-support-data-standardization/]
- 39. A proposed system for standardization of colour-coding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8630844/]
- 40. The Role of AI in Drug Discovery: Challenges, Opportunities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10302890/]
- 41. Insights on improving accessibility and usability of functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11838987/]
- 42. 6 Key Principles to Guide the Compatible Reuse of Clinical ... [https://myscrs.org/resources/reuse-clinical-data/]
- 43. Guiding Principles for Sharing Clinical Trial Data - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK285999/]
- 44. Interlaboratory evaluation of high molecular weight DNA ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11792-7]
- 45. Interrogating challenging genomic regions provides new ... [https://www.illumina.com/company/news-center/feature-articles/acmg-2025-interrogating-challenging-regions-of-the-genome.html]
- 46. Sharing Health Data Update September 2025 [https://www.healthitanswers.net/sharing-health-data-update-september-2025/]
- 47. K2 Collaborative Summit 2025 [https://klasresearch.com/report/k2-collaborative-summit-2025-connecting-payer-and-healthcare-organizations-to-improve-data-sharing-drive-efficiency-and-align-workflows/3694]
- 48. Common Issues with SEND Data Submitted for Safety ... [https://www.fda.gov/drugs/news-events-human-drugs/common-issues-send-data-submitted-safety-pharmacology-studies-11162023]
- 49. How Can Data Sharing Accelerate my Drug Research? [https://www.thermofisher.com/blog/analyteguru/how-can-data-sharing-accelerate-my-drug-research/]
- 50. Majority vote and other problems when using ... [https://pubmed.ncbi.nlm.nih.gov/24915749/]
- 51. Majority Vote and Other Problems when using... [https://www.ovid.com/journals/humm/fulltext/10.1002/humu.22600~majority-vote-and-other-problems-when-using-computational]
- 52. Rapid Whole-Genomic Sequencing and a Targeted Neonatal Gene Panel in Infants With a Suspected Genetic Disorder - PubMed [https://pubmed.ncbi.nlm.nih.gov/37432431/]
- 53. Ten simple rules for making a software tool workflow-ready [https://pmc.ncbi.nlm.nih.gov/articles/PMC8946750/]
- 54. Computational Workflows - Data Management for Research [https://guides.library.cmu.edu/researchdatamanagement/FAIR_compworkflows]
- 55. Interlaboratory variability in the measurement of direct oral anticoagulants: results from the external quality assessment scheme - PubMed [https://pubmed.ncbi.nlm.nih.gov/29322630/]
- 56. FAQ – Institute for Interlaboratory Studies [https://iisnl.com/pages/faq]
- 57. Calibrating genome wide significance by minor allele ... [https://www.nature.com/articles/s41598-025-19644-w]
- 58. Genotype-Phenotype Correlations and Putative Modifier ... [https://www.medrxiv.org/content/10.1101/2025.10.01.25336001v1]
- 59. Systematic gaps in reporting variants of uncertain ... [https://www.sciencedirect.com/science/article/pii/S1098360025001480]
- 60. The Frequency and Reclassification of Variants Uncertain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577467/]
- 61. Reassessment of variants of uncertain significance in ... [https://www.nature.com/articles/s41431-025-01911-z]
- 62. Considerations for Variants of Uncertain Significance (VUS) [https://www.rarediseasegenes.com/variants-of-uncertain-significance/]
- 63. Benchmarking computational variant effect predictors by their ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03314-7]
- 64. Benchmarking computational variant effect predictors by their ... [https://pubmed.ncbi.nlm.nih.gov/38951922/]
- 65. Variant Effect Predictors [https://www.varianteffect.org/veps/]
- 66. Essential guidelines for computational method benchmarking [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1738-8]
- 67. Recommendations for application of the functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938631/]
- 68. Variant Interpretation: Functional Assays to the Rescue - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5590843/]
- 69. Assessing In Silico Tools for Accurate Pathogenicity ... [https://www.sciencedirect.com/science/article/pii/S0022283625004796]
- 70. Evaluating variant pathogenicity prediction tools to ... [https://www.nature.com/articles/s43856-025-00883-x]
- 71. Consultation informs strategies for improving the use of ... [https://www.sciencedirect.com/science/article/pii/S0002929725001831]
- 72. Comparison of Pathogenicity Prediction Tools on Somatic ... [https://pubmed.ncbi.nlm.nih.gov/33011441/]
- 73. of locus-specific Comparison for BRCA1 and... databases [https://link.springer.com/article/10.1007/s12687-015-0220-x]
- 74. of Open-access Comparison for Clinical Databases ... Variant [https://pubmed.ncbi.nlm.nih.gov/33608312/]
- 75. Interlaboratory Comparison as a Source of Information for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8745809/]
- 76. Proficiency testing and cross-laboratory method comparison to ... [https://mbmg.pensoft.net/article/133264/]
- 77. External quality assessment and proficiency testing [https://www.pathologyoutlines.com/topic/qualityassessmentproficiencytesting.html]
- 78. Current status and future prospects of external quality ... [https://www.sciencedirect.com/science/article/pii/S3050474025000424]
- 79. Tips to Avoid Common Errors in Proficiency Testing [https://www.doctorsmanagement.com/blog/how-to-avoid-common-errors-in-proficiency-testing/]
- 80. Most Common Errors when Submitting PT Data [https://www.proficiency.org/news-press/most-common-errors-when-submitting-pt-data/]
- 81. Interpretation of EQA results and EQA-based trouble shooting [https://pmc.ncbi.nlm.nih.gov/articles/PMC5382861/]